Abstract
Purpose. The influence of different intravenous formulations on the pharmacokinetics and pharmacodynamics of propofol was investigated using the effect on the EEG (11.5-30 Hz) as pharmacodynamic endpoint.
Methods. Propofol was administered as an intravenous bolus infusion (30 mg/kg in 5 min) or as a continuous infusion (150 mg/kg in 5 hours) in chronically instrumented male rats. Propofol was formulated as a 1% emulsion in an Intralipid 10%®-like fat emulsion (Diprivan-10®, D) or as a 1%- or 6% emulsion in Lipofundin® MCT/LCT-10% (Pl% and P6%, respectively). EEG was recorded continuously and arterial blood samples were collected serially for the determination of propofol concentrations using HPLC.
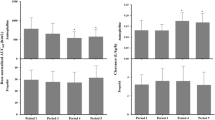
Results. Following bolus infusion, the pharmacokinetics of the various propofol emulsions could adequately be described by a two-compart-mental pharmacokinetic model. The average values for clearance (Cl), volume of distribution at steady-state (Vd,ss) and terminal half-life (t1/2, λ2) were 107 ± 4 ml/min/kg, 1.38 ± 0.06 l/kg and 16 ± 1 min, respectively (mean ± S.E., n = 22). No significant differences were observed between the three propofol formulations. After continuous infusion these values were 112 ± 11 ml/min/kg, 5.19 ± 0.41 l/kg and 45 ± 3 min, respectively (mean±S.E., n = 20) with again no statistically significant differences between the three propofol formulations. Comparison between the bolus- and the continuous infusion revealed a statistically significant difference for both Vd,ss and t1/2, λ2 (p < 0.05), whereas Cl remained unchanged. In all treatment groups infusion of propofol resulted in a burst-suppression type of EEG. A profound hysteresis loop was observed between blood concentrations and EEG effect for all formulations. The hysteresis was minimized by a semi-parametric method and resulted in a biphasic concentration-effect relationship of propofol that was described non-parametrically. For P6% a larger rate constant onset of drug effect (t,1/2, keo) was observed compared to the other propofol formulations (p<0.05).
Conclusions. The pharmacokinetics and pharmacodynamics of propofol are not affected by to a large extent the type of emulsion nor by the concentration of propofol in the intravenous formulation.
Similar content being viewed by others
REFERENCES
H. M. Bryson, B. R. Fulton, and D. Faulds. Propofol: an update on its use in anesthesia and conscious sedation. Drugs 50:513–559 (1995).
M. Lindholm. Critically ill patients and fat emulsions. Minerva. Anestesiol. 58:875–879 (1992).
V. S. Koster, J. G. Maring, C. A. J. Knibbe, R. Lange, P. F. M. Kuks, J. J. M. Langemeijer, L. P. H. J. Aarts, H. Talsma, and L. Lie-A-Huen. Propofol-6%: preparation and stability of a new formulation of propofol. J. Pharm. Sci. in press (1998).
J. Bable, A. Doenicke, and V. Monch. New formulation of propofol in an LCT/MCT emulsion: approach to reduce pain on injection. EHP 1:15–22 (1995).
A. Tibell, A. Lindholm, J. Sawe, G. Chen, and B. Norrlind. Cyclosporin A in fat emulsion carriers: experimental studies on pharmacokinetics and tissue distribution. Pharmacol. Toxicol. 76:115–121 (1995).
A. Sparreboom, O. van Tellingen, W. J. Nooijen, and J. H. Beijnen. Nonlinear pharmacokinetics of paclitaxel in mice results from the pharmaceutical vehicle Cremophor EL. Cancer Res. 56:2112–2115 (1996).
L. K. Webster, E. J. Cosson, K. H. Stokes, and M. J. Millward. Effect of the paclitaxel vehicle, Cremophor EL, on the pharmacokinetics of doxorubicin and doxorubicinol in mice. Br. J. Cancer 73:522–524 (1996).
D. J. Straathof, O. Driessen, J. W. Meijer, H. Van Rees, P. Vermeij, and T. A. Vermeij. Influence of Intralipid infusion on the elimination of phenytoin. Arch. Int. Pharmacodyn. Ther. 267:180–186 (1984).
J. W. Mandema and M. Danhof. Pharamcokinetic-pharmacodynamic modelling of the CNS effects of heptabarbital using aperiodic EEG analysis. J. Pharmacokin. Biopharm. 18:459–481 (1990).
E. H. Cox, A. G. N. Van Hemert, E. Tukker, and M. Danhof. Pharmacokinetic-pharmacodynamic modelling of the EEG effect of alfentanil. J. Pharmacol. Toxicol. Methods, 38:99–108 (1997).
C. A. J. Knibbe, V. S. Koster, V. H. M. Deneer, R. Stuurman, P. F. M. Kuks, and R. Lange. Determination of propofol in low volume samples by high-performance liquid chromatography with fluorescence detection. J. Chrom., in press (1998).
D. Verotta and L. B. Sheiner. Simultaneous modelling of pharmacokinetics and pharmacodynamics II. An improved algorithm. Comp. Applicat. Biosci. 3:345–349 (1987).
W. F. Ebling, M. Danhof, and D. R. Stanski. Pharmacodynamic characterization of the electroencephalographic effects of thiopental in J. Pharmacokin. Biopharm. 19:123–143 (1991).
B. Fulton and E. M. Sorkin. Propofol. An overview of its pharmacology and a review of its clinical efficacy in intensive care sedation. Drugs 50:636–657 (1995).
H. K. Adam, J. B. Glen, and P. A. Hoyle. Pharmacokinetics in laboratory animals of ICI 35 868, a new i.v. anaesthetic agent. Br. J. Anaesth. 52:743–746 (1980).
S. Dutta, Y. Matsumoto, and W. F. Ebling. Role of intralipid in the pharmacokinetics and pharmacodynamics of propofol in rats. Pharm. Res. 12:S401 (1995).
S. Dutta, Y. Matsumoto, N. U. Gothgen, and W. F. Ebling. Concentration-EEG effect relationship of propofol in rats. J. Pharm. Sci. 86:37–43 (1997).
I. D. Cockshott, E. J. Douglas, G. F. Plummer, and P. J. Simons. The pharmacokinetics of propofol in laboratory animals. Xenobiotica 22:369–375 (1992).
K. Leslie, D. I. Sessler, A. R. Bjorksten, and A. Moayeri. Mild hypothermia alters propofol pharmacokinetics and increases the duratio of action of atracurium. Anesth. Analg. 80:1007–1014 (1995).
J. Dingemanse, M. Danhof, and D. D. Breimer. Pharmacokinetic-pharmacodynamic modelling of CNS drug effects. An overview. Pharmacol. Ther. 38:1–52 (1988).
J. W. Mandema, E. Tukker, and M. Danhof. Pharmacokinetic-pharmacodynamic modelling of the EEG effects of midazolam in individual rats: influence of rate and route of administration. Br. J. Pharmacol. 102:663–668 (1991).
J. W. Mandema, C. D. Heijligers-Feijen, E. Tukker, A. G. De Boer, and M. Danhof. Modeling of the effect site equilibration kinetics and pharmacodynamics of racemic baclofen and its enantiomers using quantitative EEG effect measures. J. Pharmacol. Exp. Ther. 261:88–95 (1992).
K. Tomoda, K. Shingu, M. Osawa, M. Murakawa, and K. Mori. Comparison of CNS effects of propofol and thiopentone in cats. Br. J. Anaesth. 71:383–387 (1993).
K. Hartikainen, M. Rorarius, K. Makela, A. Yli-Hankala, and V. Jantti. Propofol and isoflurane induced EEG burst suppression patterns in rabbits. Acta Anaesthesiol. Scand. 39:814–818 (1995).
R. V. Reddy, S. S. Moorthy, T. Mattice, S. F. Dierdorf, and R. D. Deitch, Jr. An electroencephalographic comparison of effects of propofol and methohexital. Electroencephalogr. Clin. Neurophysiol. 83:162–168 (1992).
F. C. Forrest, M. A. Tooley, P. R. Saunders, and C. Prys-Roberts. Propofol infusion and the suppression of consciousness: the EEG and dose Br. J. Anaesth. 72:35–41 (1994).
J. W. Mandema, P. Veng-Pedersen, and M. Danhof. Estimation of amobarbital plasma-effect site equilibration kinetics. Relevance of poly-exponential conductance functions. J. Pharmacokin. Biopharm. 19:617–634 (1991).
P. Altmayer, U. Buch, and H. P. Buch. Propofol binding to human blood proteins. Arzneimittelforschung 45:1053–1056 (1995).
P. M. Klockowski and G. Levy. Kinetics of drug action in disease states. XXIII: Effect of acute hypovolemia on the pharmacodynamics of phenobarbital in. rats J. Pharm. Sci. 77:365–366 (1988).
E. Vandermeersch, J. Van Hemelrijck, G. Byttebier, and H. Van Aken. Pharmacokinetics of propofol during continuous infusion for pediatric anesthesia. Acta Anaesthesiol. Belg. 40:161–165 (1989).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Cox, E.H., Knibbe, C.A.J., Koster, V.S. et al. Influence of Different Fat Emulsion-Based Intravenous Formulations on the Pharmacokinetics and Pharmacodynamics of Propofol. Pharm Res 15, 442–448 (1998). https://doi.org/10.1023/A:1011980432646
Issue Date:
DOI: https://doi.org/10.1023/A:1011980432646