Abstract
Background: Myocardial injury and platelet activation play important roles in the pathogenesis of unstable coronary syndromes. We sought to determine whether the combined measurement of platelet and necrosis markers would improve risk stratification, and yield higher diagnostic utility in patients presenting to the emergency department with chest pain.
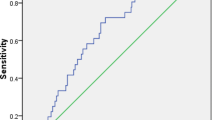
Methods and Results: Platelet and soluble P-selectin together with myoglobin, creatine kinase, CK-MB fraction, and troponin I were measured from the autologous samples in 122 consecutive patients. Statistical analysis revealed strong Spearman correlation coefficients (0.141–0.412; p<0.001) between platelet expression of P-selectin and plasma levels of necrosis markers. Platelet P-selectin and necrosis markers were independent predictors (c-index>0.7) for acute myocardial infarction, while plasma P-selectin exhibited random distribution. Elevated soluble P-selectin and myoglobin were the most valuable in identifying patients with congestive heart failure. None of the markers were useful for triaging chest pain patients with unstable angina. Analysis of incremental gains (Chi-squares) reveals that with respect to platelet P-selectin, myoglobin adds 50%% to AMI diagnostic value, and creatine kinase yields an additional 20%% in triaging these patients. The diagnostic value of soluble P-selectin is substantially (72%%) increased by myoglobin measurements, and enhanced even further (44%%) by adding cardiac troponin I for identifying heart failure patients among the chest pain population.
Conclusion: Simultaneous determination of platelet and necrosis markers improve the early diagnosis of acute myocardial infarction and congestive heart failure among patients with chest pain presenting into the Emergency Department. Well controlled clinical trials are needed to prove the advantage of combining platelet and necrosis data over presently used techniques in emergency medicine.
Similar content being viewed by others
References
Roberts R. Early diagnosis of myocardial infarction with MB CK isoforms. Clin Chim Acta 1998;272:33–45.
Millane T, Hearing SD, Jones PE, Brooks NH. Two ECGs and a history: a guide to early hospital discharge of patients with ‘chest pain cause’. J R Coll Physicians Lond 1998;32:122–124.
Hedges JR, Young GP, Henkel GF, Gibler WB, Green TR, Swanson JR. Serial ECGs are less accurate than serial CK-MB results for emergency department diagnosis of myocardial infarction. Ann Emerg Med 1992;21:1445–1450.
de Winter RJ, Koster RW, Sturk A, Sanders GT. Value of myoglobin, troponin T, and CK-MB mass in ruling out an acute myocardial infarction in the emergency room. Circulation 1995;92:3401–3407.
Kontos MC, Arrowood JA, Paulsen WH, Nixon JV. Early echocardiography can predict cardiac events in emergency department patients with chest pain. Ann Emerg Med 1998;31:550–557.
Mair J. Glycogen phosphorylase isoenzyme BB to diagnose ischaemic myocardial damage. Clin Chim Acta 1998;272:79–86.
Falahati A, Sharkey SW, Christensen D, McCoy M, Miller EA, Murakami MA, Apple FS. Implementation of serum cardiac troponin I as marker for detection of acute myocardial infarction. Am Heart J 1999;137:332–337.
Zimmerman J, Fromm R, Meyer D, et al. Diagnostic marker cooperative study for the diagnosis of myocardial infarction. Circulation 1999;99:1671–1677.
Puleo PR, Meyer D, Wahten C, et al. Use of a rapid assay of subforms of creatine kinase MB to diagnose or rule out acute myocardial infarction. N Engl J Med 1994;331:561–566.
Hollander JE, Muttreja MR, Dalesandro MR, Shofer FS. Risk stratification of emergency department patients with acute coronary syndromes using P-selectin. J Am Coll Cardiol 1999;34:95–105.
Gurbel PA, Kereiakes DJ, Dalesandro MR, Bahr RD, O'Connor CM, Serebruany VL. The role of soluble and platelet-bound P-selectin in discriminating cardiac from non-cardiac chest pain at presentation in the emergency department. Amer Heart J 2000;(in press).
Serebruany VL, Kereiakes DJ, Dalesandro MR, Gurbel PA. Model of flow cytometer markedly affects platelet-bound P-selectin expression in patients with chest pain. Are we comparing apples with oranges? Thromb Res 1999;96:51–56.
Hanley JA, McNeil BJ. The meaning and use of the area under the receiver operating characteristic (ROC) curve. Radiology 1982;143:29–36.
World Health Organization. Report of the Joint International Society and Federation of Cardiology/World Health Organization Task Force on Standardization of Clinical Nomenclature. Nomenclature and criteria for diagnosis of ischemic heart disease. Circulation 1979;59:607–609.
Lee TH, Weisberg MC, Brand DA, Rouan GW, Goldman L. Candidates for thrombolysis among emergency room patients with acute chest pain: potential true-and false-positive rates. Ann Intern Med 1989;110:957–962.
Weingarten SR, Ermann B, Riedinger MS, Shah PK, Ellrodt AG. Selecting the best triage rule for patients hospitalized with chest pain. Am J Med 1989;87:494–500.
Rozenman Y, Gotsman MS. The earliest diagnosis of acute myocardial infarction. Ann Rev Med 1994;45:31–44.
Ryan TJ, Anderson JL, Antman EM, et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction). J Am Coll Cardiol 1996;28:1328–1428.
The Cardiology Roundtable: Perfecting MI ruleout. Best practices for emergency evaluation of chest pain. Washington, DC: The Advisory Board Co., 1994:15.
Christenson RH, Newby LK, Ohman EM. Cardiac markers in the assessment of acute coronary syndromes. Md Med J 1997;Suppl:18–24.
Katus HA, Diederich KW, Scheffold T, Vellner M, Schwarz F, Kubler W. Non-invasive assessment of infarct reperfusion: the predictive power of the time to peak value of myoglobin, CKMB, and CK in serum. Eur Heart J 1998;9:619–624.
Pumphrey CW, Dawes J. Plasma beta-thromboglobulin as a measure of platelet activity. Effect of risk factors and findings in ischemic heart disease and after acute myocardial infarction. Am J Cardiol 1982;50:1258–1261.
Hughes A, Daunt S, Vass G, Wickes J. In vivo platelet activation following myocardial infarction and acute coronary ischemia. Thromb Haemost 1982;48:133–135.
Ikeda H, Takajo Y, Ichiki K, et al. Increased soluble form of P-selectin in patients with unstable angina. Circulation 1995;92:1693–1696.
Verhaar MC, Beutler JJ, Gaillard CA, Koomans HA, Fijnheer R, Rabelink TJ. Progressive vascular damage in hypertension is associated with increased levels of circulating P-selectin. J Hypertens 1998;16:45–50.
Kaikita K, Ogawa H, Yasue H, et al. Soluble P-selectin is released into the coronary circulation after coronary spasm. Circulation 1995;92:1726–1730.
Gurbel PA, Serebruany VL. Myths and realities of plasma P-selectin levels in patients with acute myocardial infarction. Thromb Res 1997;88:343–344.
Langford EJ, Wainwright RJ, Martin JF. Platelet activation in acute myocardial infarction and unstable angina is inhibited by nitric oxide donors. Arterioscl Thromb Vasc Biol 1996;16:51–55.
Becker RC, Tracy RP, Bovill EG, Mann KG, Ault K. The clinical use of flow cytometry for assessing platelet activation in acute coronary syndromes. TIMI-III Thrombosis and Anticoagulation Group. Cor Artery Dis 1994;5:339–345.
Tenaglia N, Buda AJ, Wilkins RG, et al. Levels of expression of P-selectin, E-selectin, and intercellular adhesion molecule-1 in coronary atherectomy specimens from patients with stable and unstable angina pectoris. Am J Cardiol 1997;79:742–747.
Christenson RH, Azzazy HM. Biochemical markers of the acute coronary syndromes. Clin Chem 1998;44:1855–1864.
Knight CJ, Panesar M, Wright C, et al. Altered platelet function detected by flow cytometry. Effects of coronary artery disease and age. Arterioscler Thromb Vasc Biol 1997;17:2044–2053.
Taggart DP, Hadjinikolas L, Hooper JM, et al. Effects of age and ischemic times on biochemical evidence of myocardial injury after pediatric cardiac operations. J Thor Cardiovasc Surg 1997;113:728–735.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Serebruany, V.L., Levine, D.J., Nair, G.V. et al. Usefulness of Combining Necrosis and Platelet Markers in Triaging Patients Presenting with Chest Pain to the Emergency Department. J Thromb Thrombolysis 11, 155–162 (2001). https://doi.org/10.1023/A:1011280801335
Issue Date:
DOI: https://doi.org/10.1023/A:1011280801335