Abstract
Rationale
Disruption in cognition is characteristic of psychiatric illnesses such as schizophrenia. Studies of drugs that improve cognition might provide a better insight into the mechanisms underlying cognitive deficits.
Objectives
We compared the effects of the antipsychotic drugs aripiprazole, olanzapine, and haloperidol on performance deficit in a test of divided and sustained visual attention, the five-choice serial reaction time task (5-CSRTT), which provides information on attentional functioning (accuracy of visual discrimination), response control (measured by anticipatory and perseverative responses) and speed.
Methods
The cognitive deficit was induced by infusion of the competitive NMDA receptor antagonist 3-(R)-2-carboxypiperazin-4-propyl-1-phosphonic acid (CPP) in the rat medial prefrontal cortex (mPFC). In vivo microdialysis was used to compare the effects of aripiprazole, olanzapine and haloperidol on CPP-induced glutamate (GLU) and serotonin (5-HT) release in the mPFC of conscious rats.
Results
Oral aripiprazole (1.0 and 3.0 mg/kg) and olanzapine (0.3 and 1.0 mg/kg), but not haloperidol (0.1 mg/kg), abolished the CPP-induced accuracy deficit and GLU release. Haloperidol and aripiprazole, but not olanzapine, reduced perseverative over-responding, while anticipatory responding was best controlled by olanzapine. However, these effects were not associated with changes in GLU release. No association was found between the effects of these antipsychotics on CPP-induced attentional performance deficits in the 5-CSRTT and 5-HT efflux.
Conclusions
The data confirm that excessive GLU release in the mPFC is associated with attentional deficits. Thus, suppression of GLU release may be a target for the development of novel antipsychotic drugs with greater effect on some aspects of cognitive deficits.
Similar content being viewed by others
Introduction
One widely used model of cognitive impairments in schizophrenia focuses on disturbances in N-methyl-d-aspartate (NMDA) receptor-mediated glutamate (GLU) neurotransmission in the medial prefrontal cortex (mPFC; Javitt and Zukin 1991; Moghaddam and Jackson 2003). Disinhibition of GLU transmission may account for the increase in human frontal cortex metabolism and resting cerebral blood flow after ketamine (Breier et al. 1997; Holcomb et al. 2005; Vollenweider et al. 1997b). In rats, the disruptive effects of acute NMDA receptor antagonists on motor activity, working memory, and attention may be associated with the ability to raise extracellular GLU concentrations in the mPFC (Ceglia et al. 2004; Mirjana et al. 2004; Moghaddam et al. 1997; Moghaddam and Adams 1998).
It has been suggested that serotonergic mechanisms, particularly those dependent on 5-HT1A and 5-HT2A receptors, play a key role in psychosis, cognition, mood, and treatment response in schizophrenia through their influence on GLU neurotransmission (Aghajanian and Marek 2000). Specifically, NMDA receptor antagonists or genetic deletion of the NMDA receptors raises 5-HT release in the mPFC (Amargos-Bosch et al. 2005; Ceglia et al. 2004; Miyamoto et al. 2001), whereas activation of 5-HT2A receptors raises cortical GLU release (Scruggs et al. 2003), enhances GLU-dependent excitatory postsynaptic currents in cortical slices (Aghajanian and Marek 1999) and c-fos expression (Scruggs et al. 2000) in the mPFC. The 5-HT1A receptors mediate the hyperpolarizing action of 5-HT on glutamatergic prefrontal neurons (Aghajanian and Marek 1997; Amargos-Bosch et al. 2004; Zhou and Hablitz 1999).
Aripiprazole is a new antipsychotic drug with a pharmacological profile different from the conventional and atypical antipsychotics. It is a partial agonist at 5-HT1A and antagonist at 5-HT2A receptors, but unlike other antipsychotics, which are potent D2 receptor antagonists, aripiprazole has partial agonist activity on these receptors (Burris et al. 2002; Jordan et al. 2002a, b). The drug is effective in different animal models of psychosis (Morimoto et al. 2002) as well as in some models of negative symptoms (Bruins Slot et al. 2005; Snigdha and Neill 2008). However, its efficacy in animal models of cognitive deficits is not yet clear.
The five-choice serial reaction time task (5-CSRTT) has clear links with its human analog, the continuous performance test used to assess attention and vigilance in schizophrenic patients. Optimal performance in this task requires the integration of a number of component cognitive processes such as sustained and selective attention and response control. The task provides different and, to some extent, independent measures of aspects of selective attention (measured by accuracy of detection) and inhibitory response control, such as impulsive (anticipatory) and compulsive (perseverative) responding, as well as speed of responding and motivation. It therefore permits direct comparison of the effects of selective manipulation of neurotransmission on these different cognitive processes (Robbins 2002).
Antipsychotics are poorly effective against neurocognitive disturbances of schizophrenia, and it is highly controversial whether there are any differences between novel and older drugs (Green et al. 2002; Keefe et al. 2004, 2007). However, atypical antipsychotics with high affinity for 5-HT receptors appear somewhat more effective in improving certain aspects of cognitive deficits (Harvey and Keefe 2001; Keefe et al. 1999, 2004; Meltzer and McGurk 1999). Differences between the effects of conventional and atypical antipsychotics have also been observed in NMDA receptor antagonist-based animal models of cognitive deficits of schizophrenia (Amitai et al. 2007; Bakshi et al. 1994; Baviera et al. 2008; Hoffman et al. 1993; Rodefer et al. 2008) and on spontaneous and dizocilpine-induced activity of mPFC neurons (Homayoun and Moghaddam 2007b) and GLU and 5-HT release in the rat mPFC (Lopez-Gil et al. 2009).
As drugs preventing the impairment in attention induced by intra-mPFC 3-(R)-2-carboxypiperazin-4-propyl-1-phosphonic acid (CPP) suppress GLU release in the mPFC (summarized in Table 1), we hypothesized that aripiprazole might prevent attentional deficits and the release of GLU induced by NMDA receptor blockade. The present study is therefore aimed at assessing the effects of aripiprazole on intra-mPFC CPP-induced attentional deficits in the 5-CSRTT and on GLU and 5-HT release in the mPFC, as measured by in vivo microdialysis in conscious rats. The effects of olanzapine and haloperidol, an atypical and a typical antipsychotic drug, respectively, were also examined.
Materials and methods
Animals
Male Lister hooded rats (Charles River, Calco, Italy) weighing about 250–300 g were used. They were housed at a constant room temperature (22 ± 1°C), with relative humidity 50 ± 10%, and a 7 a.m.–7 p.m. day/night cycle. Different batches of rats were used for behavioral and microdialysis studies. Food was freely available for rats used in microdialysis experiments, but access was limited for rats used in behavioral experiments (about 15 g of Altromin pellets per rat, at the end of each day’s testing, to keep the animals at 85–90% of their initial free-feeding weight). Water was available ad libitum.
All experiments were conducted in conformity with the institutional guidelines that are in compliance with national (D.L. n. 116, G.U., Suppl. 40, 18 Febbraio 1992, Circolare No. 8, G.U., 14 Luglio 1994) and international laws and policies (EEC Council Directive 86/609, OJ L 358, 1, Dec.12, 1987; Guide for the Care and Use of Laboratory Animals, US National Research Council, 1996).
Behavioral studies
Five-choice serial reaction time task (5-CSRTT)
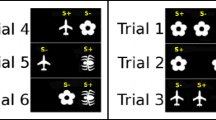
The apparatus consisted of four specially designed boxes (Campden Ins. UK) controlled online by Whisker software (Cambridge University Technical Services, UK). The apparatus and training procedures have been described elsewhere (Carli et al. 1983).
Briefly, rats were trained to wait for a fixed time (5 s) before a brief visual stimulus (0.5 s) was presented in one of the five holes. The light was on, and for a short period afterwards (limited hold), a response in the hole that was illuminated (correct response) resulted in the delivery of a food pellet. Responses in the holes that had not been illuminated (incorrect responses) or failure to respond within the limited hold (omissions) caused the houselight to be turned off for a short period (time out). Throughout the study, each rat had only one session consisting of 100 trials/day.
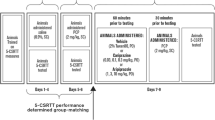
A number of performance measures were recorded including choice accuracy (the proportion of correct responses to the total number of correct plus incorrect responses), proportion of omissions (the number of omissions to the total number of correct + incorrect + omissions), anticipatory responses (responses made in the holes during the waiting period before presentation of the target), perseverative responses (responses repeated in the holes after a correct response but before collecting the food pellet). Correct response latency (the time from the stimulus onset to a correct response) and magazine latency (the time from the correct response to the collection of food from the magazine) were also recorded. A total of 30 rats were trained on the 5-CSRT task, and they all reached the criterion of about 80% correct responses with no more than 20% omissions before surgery and pharmacological experiments. As shown in Fig. 1, the tree groups had similar accuracy and omissions under vehicle injections. The percentages of correct responses were: aripiprazole 90.9 ± 1.73, olanzapine 85.7 ± 2.05, and haloperidol 85.5 ± 1.49. The percentages of omissions were: aripiprazole 15.0 ± 1.65, olanzapine 15.9 ± 3.36, and haloperidol 11.7 ± 1.38.
The effects of aripiprazole, olanzapine, and haloperidol on the accuracy of visual discrimination, measured by the percentage of correct responses. Vehicle (0; 2 ml/kg) or aripiprazole (1.0 and 3.0 mg/kg), olanzapine (0.1, 0.3, and 3.0 mg/kg), and haloperidol (0.1 mg/kg) were administered orally. Fifty minutes later, rats received bilateral injections of vehicle (VEHICLE; 1 μl) or CPP (50 ng/μl/side) into the mPFC and 10 min later started the test session. The various treatment combinations were administered at least 48 h apart according to a Latin-square design. The histograms represent the mean ± SEM of 8 (aripiprazole), 10 (olanzapine), and 9 (haloperidol) rats. *P < 0.05 vs. VEHICLE (0); #P < 0.05 vs. CPP (0; Tukey’s test)
Surgery, drug administration, and microinjection procedure
Rats previously trained to a stable level of performance were anesthetized by an intraperitoneal (IP) injection (2 ml/kg) of 40 mg/ml ketamine and 5 mg/ml xylazine. All animals received 0.1 mg/kg atropine sulfate IP. The rats were secured in a stereotaxic frame (Kopf Instruments, USA) with the incisor bar set at −3.3 mm relative to the interaural line. Bilateral 23-gauge, stainless steel guide cannulas (Cooper’s Needles, UK) were implanted in the mPFC using standard stereotaxic techniques. The coordinates referred to the tip of the implanted cannulas were: AP +3.7 mm from bregma, L ±0.7 mm from midline, and DV −2.8 from dura (Paxinos and Watson 1986). Stainless steel stylets (30 gauge) were inserted flush with the end of the guide cannulas. The tip of injection needle protruded 2 mm below the cannulas tip, thus reaching a DV of −4.8 mm, which is similar to the DV coordinate of the probe tip in microdialysis experiments.
On each test day, rats were given aripiprazole (1.0 and 3.0 mg/kg), olanzapine (0.1, 0.3 and 1.0 mg/kg), haloperidol (0.1 mg/kg), or 2 ml/kg vehicle by oral gavage. Fifty minutes later, while the rat was held, the stylets were removed and two injection units terminating 2 mm below the tip of the guides were inserted. One microliter per hemisphere of CPP (50 ng/μl) or vehicle was delivered into the mPFC, at a rate of 0.5 μl/min, with a 10-μl syringe mounted in a CMA/100 infusion pump (CMA Microdialysis, Sweden) connected by PE10 tubing to the injection units, which were left in place for 1 min to allow for diffusion.
Microdialysis studies
A total of 90 behaviorally naive Lister hooded rats were used for microdialysis studies.
Surgery and microdialysis procedures
Concentric dialysis probes were made with Cuprophan membrane (216-μm outer diameter, 3,000 Da cutoff, Sorin Biomedica, Italy), essentially as described elsewhere (Robinson and Whishaw 1988). The membrane exposed to the brain tissue was 4 mm long. Rats were anesthetized with 3 ml/kg IP equithesin (composition in mM: pentobarbital 39, chloral hydrate 256, MgSO4 86, ethanol 10% v/v, propylene glycol 39.6% v/v), then positioned on a stereotaxic frame (Kopf Instruments), and a dialysis probe was implanted in the mPFC. The stereotaxic coordinates referred to the tip of the probe were: AP +3.7 and L ±0.7 mm from bregma and DV −4.8 mm from dura surface (Paxinos and Watson 1986). About 20 h after surgery, the probes were perfused with artificial cerebrospinal fluid (aCSF, composition in mM: NaCl 140, CaCl2 1.26, KCl 3, MgCl2 1, Na2HPO4 1.2, glucose 7.2; pH 7.4 with 0.6 M NaH2PO4) at 1 μl/min with a CMA/100 pump (CMA Microdialysis). Once the extracellular GLU and 5-HT concentrations were stable (at least three consecutive samples differing less than 20% from the mean basal value), rats were given aripiprazole, olanzapine, haloperidol, or vehicle by oral gavage. After 60 min, 100 μM CPP dissolved in aCSF was infused through the probe for 2 h. Samples of dialysate were collected every 20 min and stored at 4°C.
Chromatographic analysis
Concentrations of GLU and 5-HT in the dialysate were measured by high-performance liquid chromatography coupled to fluorometric or electrochemical detection, as previously described (Ceglia et al. 2004).
Histology
At the end of behavioral and neurochemical experiments, rats were deeply anesthetized with chloral hydrate (400 mg/kg IP) and killed by decapitation. The brain was removed and frozen on dry ice. Correct probe and cannula placement was checked by visual inspection of the tracks on 30-μm coronal sections. Only rats with correct cannula and probe placements were included in the results (86 out of 90 in microdialysis studies). The rats excluded from behavioral data due to misplacement of the injection cannulas were: one in the haloperidol, none in the olanzapine, and two in the aripiprazole group.
Drugs
Both microdialysis and behavioral experiments used 3-(R)-2-carboxypiperazin-4-propyl-1-phosphonic acid (CPP; Tocris, USA) dissolved in saline or aCSF. Aripiprazole (Bristol-Myers Squibb, Italy), olanzapine (Eli Lilly, USA), haloperidol (Lusofarmaco, Italy), and vehicle were given orally 60 min before the infusion of CPP. The dose/concentration of CPP used in behavioral and microdialysis studies was respectively those shown to produce attention impairment and increase extracellular GLU in the mPFC (Ceglia et al. 2004; Mirjana et al. 2004). The doses of antipsychotics were selected on the basis of their ability to reverse apomorphine-induced hypermotility (Kikuchi et al. 1995; Morimoto et al. 2002). The drugs were dissolved in 90% lactic acid (15–250 μl), diluted with sterile water, and the pH of the solutions was adjusted to 4.0–5.5 with 5 M NaOH. Control rats received the same volume of acidified water.
Statistics
Microdialysis
Extracellular levels of GLU were expressed as percentages of basal values and analyzed by analysis of variance (ANOVA) for repeated measures with treatments (CPP, aripiprazole, olanzapine, and haloperidol) as the between-subject factor and time as the within-subject factor. In rats given CPP alone or in combination with antipsychotic drugs, the analysis was applied to the part of the curve from 60 to 180 min, corresponding to the duration of the CPP infusion. Post hoc comparisons were done with Tukey–Kramer’s test. For the sake of clarity, the effects of antipsychotics alone were shown in separate figures.
Behavioral studies
The effects of aripiprazole (n = 8), olanzapine (n = 10), and haloperidol (n = 9) on CPP-induced attentional performance deficits were tested in three groups of rats. Only the data for 0.1 mg/kg haloperidol were analyzed; a higher dose (0.3 mg/kg) was also administered, but as the majority of rats stopped responding, the data were not reliable and were not analyzed. The effects of CPP in combination with aripiprazole, olanzapine, or haloperidol on (a) the percentage of correct responses, (b) the percentage of omissions, (c) the mean correct response latency, (d) the number of anticipatory responses, and (e) the number of perseverative responses were analyzed by repeated-measure two-way ANOVA with factors haloperidol, olanzapine, or aripiprazole and CPP. The means of the individual treatment combinations were compared by Tukey’s honestly significant difference test.
Results
Effects on accuracy
The effects of aripiprazole, olanzapine, and haloperidol on CPP-induced impairment of the accuracy of visual discrimination (measured by the percentage of correct responses) in the 5-CSRTT are shown in Fig. 1. Injected bilaterally into the mPFC, 50 ng/μl CPP reduced accuracy in all the three groups of rats. Oral pretreatment with aripiprazole abolished the CPP-induced loss of accuracy (aripiprazole × CPP: F 2,35 = 6.8, P = 0.003; CPP: F 1,35 = 13.3, P = 0.0008; aripiprazole: F 2,35 = 2.1, P > 0.05). Aripiprazole doses of 1 and 3 mg/kg were equally effective in restoring normal levels of accuracy (both doses of aripiprazole plus CPP compared to vehicle plus CPP, P < 0.05). Similarly, oral pretreatment with olanzapine reduced the impairment in accuracy (olanzapine × CPP: F 3,63 = 2.8, P = 0.04; CPP: F 3,63 = 59.8, P ≤ 0.0001; olanzapine: F 3,63 = 4.4, P = 0.007). Although olanzapine dose-dependently boosted the accuracy of CPP-injected rats, Tukey’s test indicated that the effect was significant only at 1.0 mg/kg (olanzapine 0.1 or olanzapine 0.3 plus CPP compared to vehicle plus CPP, P > 0.05; olanzapine 1.0 plus CPP compared to vehicle plus CPP, P < 0.05). In contrast, oral pretreatment with 0.1 mg/kg haloperidol was unable to reverse the CPP-induced impairment in accuracy (haloperidol × CPP: F 1,24 = 1.9, P > 0.05; CPP: F 1,24 = 8.9, P = 0.006; haloperidol: F 1,24 = 0.1, P > 0.05). As there was no significant interaction between haloperidol and CPP or main effect of haloperidol on accuracy, no further analysis of treatment means was done.
No dose of aripiprazole, olanzapine, or haloperidol had any effect on accuracy on its own (comparison with vehicle plus vehicle, all P > 0.05; Tukey’s test).
Effects on impulsivity
As shown in Fig. 2, intracortically injected CPP substantially increased impulsivity, as measured by the number of anticipatory responses. Although all three antipsychotics reduced this impulsivity, the effects were statistically significant only for olanzapine and haloperidol. Two-way repeated-measure ANOVA showed a significant effect of haloperidol (haloperidol × CPP: F 1,24 = 5.8, P = 0.02; CPP: F 1,24 = 5.8, P = 0.02; haloperidol: F 1,24 = 5.8, P = 0.02) and olanzapine (olanzapine × CPP: F 3,63 = 3.2, P = 0.02; CPP: F 1,63 = 78.3, P ≤ 0.0001; olanzapine: F 3,63 = 1.2, P > 0.05), but not aripiprazole (aripiprazole × CPP: F 2,35 = 1.6, P > 0.05; CPP: F 1,35 = 9.2, P = 0.004; aripiprazole: F 2,35 = 4.9, P = 0.02). Further analyses comparing the treatment means showed that CPP-injected rats made fewer anticipatory responses after 0.1, 0.3, or 1.0 mg/kg olanzapine (each dose of olanzapine plus CPP compared to vehicle plus CPP, P < 0.05). A similar decrease was seen when CPP-injected rats were pretreated with 0.1 mg/kg haloperidol (haloperidol 0.1 plus CPP compared to vehicle plus CPP, P < 0.05). Aripiprazole also lowered the number of anticipatory responses made by CPP-injected rats (Fig. 2). However, Tukey’s test indicated that the decreases were not significant (both doses of aripiprazole plus CPP compared to vehicle plus CPP, P > 0.05). Olanzapine, but not aripiprazole, or haloperidol reduced the impulsivity of vehicle-injected rats (compared to vehicle plus vehicle, P < 0.05).
The effects of aripiprazole, olanzapine, and haloperidol on impulsivity, measured by the number of anticipatory responses. Vehicle (0; 2 ml/kg) or aripiprazole (1.0 and 3.0 mg/kg), olanzapine (0.1, 0.3, and 3.0 mg/kg), and haloperidol (0.1 mg/kg) were administered orally. Fifty minutes later, rats received bilateral injection of vehicle (VEHICLE; 1 μl) or CPP (50 ng/μl/side) into the mPFC and 10 min later started the test session. The various treatment combinations were administered at least 48 h apart according to a Latin-square design. The histograms represent the mean ± SEM of 8 (aripiprazole), 10 (olanzapine), and 9 (haloperidol) rats. *P < 0.05 vs. VEHICLE (0); #P < 0.05 vs. CPP (0; Tukey’s test)
Effects on perseverative responding
Intracortical injections of CPP raised the number of perseverative responses, and this effect was abolished by aripiprazole and haloperidol, but not olanzapine (Fig. 3).
The effects of aripiprazole, olanzapine, and haloperidol on compulsivity, measured by the number of perseverative responses. Vehicle (0; 2 ml/kg) or aripiprazole (1.0 and 3.0 mg/kg), olanzapine (0.1, 0.3, and 3.0 mg/kg), and haloperidol (0.1 mg/kg) were administered orally. Fifty minutes later, rats received bilateral injection of vehicle (VEHICLE; 1 μl) or CPP (50 ng/μl/side) into the mPFC and 10 min later started the test session. The various treatment combinations were administered at least 48 h apart according to a Latin-square design. The histograms represent the mean ± SEM of 8 (aripiprazole), 10 (olanzapine), and 9 (haloperidol) rats. *P < 0.05 vs. VEHICLE (0); #P < 0.05 vs. CPP (0; Tukey’s test)
As shown by two-way repeated-measure ANOVA, aripiprazole (aripiprazole × CPP: F 2,35 = 3.8, P = 0.04; aripiprazole: F 2,35 = 2.9, P > 0.05; CPP: F 1,35 = 16.3, P = 0.0003) and haloperidol (haloperidol × CPP: F 1,24 = 8.4, P = 0.008; haloperidol: F 1,24 = 9.0, P = 0.006; CPP: F 1,24 = 42.3, P < 0.0001) both prevented CPP’s effect on perseverative responses. Pretreatment with olanzapine had no such effect (olanzapine × CPP: F 3,63 = 0.3, P > 0.05; olanzapine: F 3,63 = 1.2, P > 0.05; CPP: F 1,63 = 62.8, P ≤ 0.0001).
Both doses of aripiprazole prevented the increase in perseverative responding induced by CPP, but the effect was statistically significant only with 3.0 mg/kg (aripiprazole 1.0 plus CPP compared to vehicle plus CPP, P > 0.05; aripiprazole 3.0 plus CPP compared to vehicle plus CPP, P < 0.05). Similarly, 0.1 mg/kg of haloperidol prevented the increase in perseverative responding (haloperidol 0.1 plus CPP compared to vehicle plus CPP, P < 0.05). No dose of olanzapine reduced CPP’s effects on perseverative over-responding (each dose of olanzapine plus CPP compared to vehicle plus CPP, P > 0.05). The various doses of aripiprazole, olanzapine, or haloperidol in vehicle-injected rats had no effect on perseverative responding.
CPP increased the percentage of omissions and latencies to make a correct response and to collect food reward, but none of the drug alone had any effect or prevented the effects of CPP (data not shown).
Basal GLU and 5-HT
Basal extracellular concentrations of GLU and 5-HT in the mPFC were respectively 27.8 ± 1.5 pmol/20 μl (n = 86) and 5.6 ± 0.3 fmol/20 μl (n = 82). These values were not corrected for in vitro recovery of the probes.
Effects of aripiprazole, olanzapine, and haloperidol on basal and CPP-induced release of GLU
Figure 4 shows the effects of aripiprazole, olanzapine, and haloperidol on the rise of extracellular GLU induced by CPP. CPP 100 μM infused through the probe increased extracellular GLU, reaching 240% of basal values 40 min after the start of the infusion and remaining above control values until the end of the infusion.
Effects of aripiprazole (ARI), olanzapine (OLA), haloperidol (HAL), and vehicle (VEH) on CPP-induced GLU release in the mPFC. Drugs and vehicle were given orally (arrows) 60 min before the infusion of 100 μM CPP through the probe (horizontal bar). The doses (mg/kg) are indicated in parentheses. The VEH + VEH and VEH + CPP groups in the center and right panels (dotted lines) are the same as in the left panel. Data are expressed as percentages of basal values and are the mean ± SEM of 5–8 rats/group. #P < 0.05, ARI (1.0) + CPP, OLA (0.3) + CPP, and HAL (0.1) + CPP vs. VEH + CPP; *P < 0.05, ARI (3.0) + CPP, OLA (1.0) + CPP, and HAL (0.3) + CPP vs. VEH + CPP (Tukey’s test)
Pretreatment with aripiprazole abolished the CPP-induced rise of extracellular GLU. ANOVA indicated a significant interaction between aripiprazole and CPP (F 2,31 = 6.7, P = 0.004), but no effect of aripiprazole (F 2,31 = 0.7, P = 0.5) and CPP (F 1,31 = 3.1, P = 0.09). Post hoc analysis using Tukey’s test showed that extracellular GLU in rats given 1.0 and 3.0 mg/kg aripiprazole was significantly lower than in those receiving CPP alone (both doses of aripiprazole plus CPP vs. CPP alone, P < 0.05) and not significantly different from those given vehicle (P > 0.05).
Olanzapine abolished the effect of CPP on extracellular GLU (olanzapine × CPP: F 2,33 = 5.7, P = 0.008; CPP: F 1,33 = 17.4, P = 0.0002; olanzapine: F 2,33 = 1.5, P = 0.2). Post hoc analysis showed that both doses (0.3 and 1.0 mg/kg) suppressed CPP’s effect on extracellular GLU.
Haloperidol had opposite effects on the CPP-induced rise of extracellular GLU, depending on the dose (haloperidol × CPP: F 2,30 = 6.8, P = 0.004; CPP: F 1,30 = 39.0, P < 0.0001; haloperidol: F 2,30 = 6.8, P = 0.004). At 0.1 mg/kg, haloperidol significantly enhanced the rise of extracellular GLU, while at 0.3 mg/kg, it abolished it.
As shown in Fig. 5, by themselves, aripiprazole and haloperidol had no significant effects on extracellular GLU (aripiprazole: F 2,13 = 0.8, P = 0.5; aripiprazole × time: F 18,117 = 0.9, P = 0.6; haloperidol: F 2,14 = 0.6, P = 0.6; haloperidol × time: F 18,126 = 0.5, P = 0.93).
Effects of aripiprazole (ARI), olanzapine (OLA), haloperidol (HAL), and vehicle (VEH) on basal GLU release in the mPFC. Arrows indicate the oral administration of drugs or vehicle. The doses (mg/kg) are indicated in parentheses. The VEH + VEH group was the same as in Fig. 4. Data are expressed as percentages of basal values and are the mean ± SEM of 5–6 rats/group. *P < 0.05, OLA + VEH vs. VEH + VEH (Tukey’s test)
Extracellular GLU in rats given 1.0 mg/kg olanzapine were significantly higher than in those receiving vehicle (147% of basal values at 100 min), while 0.3 mg/kg olanzapine had no significant effect. ANOVA showed a significant effect of olanzapine (F 2,14 = 6.7, P = 0.01) and olanzapine × time interaction (F 18,126 = 1.8, P = 0.03).
Effects of aripiprazole, olanzapine, and haloperidol on basal and CPP-induced rise of extracellular 5-HT
Figures 6 and 7 show the effects of aripiprazole, olanzapine, and haloperidol on basal extracellular 5-HT in the mPFC and the CPP-induced rise. Extracellular 5-HT reached 180% of basal values 60 min after the start of CPP infusion in vehicle pretreated rats. The effect was abolished by aripiprazole (aripiprazole × CPP: F 2,27 = 10.6, P = 0.0004; CPP: F 1,270 = 3.1, P = 0.09; aripiprazole: F 2,27 = 4.3, P = 0.02). Post hoc analysis showed that 1.0 and 3.0 mg/kg aripiprazole both suppressed the rise of extracellular 5-HT.
Effects of aripiprazole (ARI), olanzapine (OLA), haloperidol (HAL), and vehicle (VEH) on CPP-induced 5-HT release in the mPFC. Drugs and vehicle were given orally (arrows) 1 h before the infusion of 100 μM CPP through the probe (horizontal bar). The VEH + VEH and VEH + CPP groups in the center and right panels (dotted lines) are the same as in the left panel. The doses (mg/kg) are indicated in parentheses. Data are expressed as percentages of basal values and are the mean ± SEM of 5–7 rats/group. #P < 0.05, ARI (1.0) + CPP, OLA (0.3) + CPP, and HAL (0.1) + CPP vs. VEH + CPP; *P < 0.05, ARI (3.0) + CPP and HAL (0.3) + CPP vs. VEH + CPP (Tukey’s test)
Effects of aripiprazole (ARI), olanzapine (OLA), haloperidol (HAL), and vehicle (VEH) on basal 5-HT release in the mPFC. Arrows indicate the oral administration of drugs or vehicle. The doses (mg/kg) are indicated in parentheses. The VEH + VEH group was the same as in Fig. 6. Data are expressed as percentages of basal values and are the mean ± SEM of 5–6 rats/group. *P < 0.05, ARI (3.0) + VEH vs. VEH + VEH; or HAL (0.1) + VEH vs. VEH + VEH (Tukey’s test)
ANOVA showed an overall significant effect of olanzapine on the CPP-induced rise of extracellular 5-HT (olanzapine × CPP: F 2,30 = 3.3, P = 0.05; CPP: F 2,30 = 0.5, P = 0.5; olanzapine: F 2,30 = 0.8, P = 0.5). However, post hoc analysis showed that 0.3 mg/kg suppressed the effect, but 1.0 mg/kg did not.
At 0.1 and 0.3 mg/kg, haloperidol completely suppressed the rise of extracellular 5-HT (haloperidol × CPP: F 2,29 = 3.3, P = 0.05; CPP: F 1,29 = 15.9, P = 0.0004; haloperidol: F 2,29 = 10.1, P = 0.0005).
At 1.0 mg/kg, aripiprazole, by itself, had no effect on extracellular 5-HT, while at 3.0 mg/kg, it significantly increased extracellular 5-HT, reaching 149% of basal values at 140 min (aripiprazole: F 2,12 = 13.8, P = 0.0008; time: F 9,18 = 2.3, P = 0.02; aripiprazole × time: F 18,108 = 1.8, P = 0.03). Olanzapine also had no effect on extracellular 5-HT (olanzapine: F 2,12 = 1.9, P = 0.2; time: F 9,18 = 1.7, P = 0.1; olanzapine × time: F 18,108 = 0.8, P = 0.7). By itself, 0.1 mg/kg haloperidol reduced extracellular 5-HT (74% of basal values), while 0.3 mg/kg had no effect (haloperidol: F 2,14 = 13.8, P = 0.0008; time: F 9,18 = 2.1, P = 0.03; haloperidol × time: F 18,126 = 1.1, P = 0.4).
Discussion
The present data show that aripiprazole and olanzapine abolished the CPP-induced accuracy impairment in the 5-CSRTT, while haloperidol had no effect. Interestingly, haloperidol and aripiprazole, but not olanzapine, reduced perseverative over-responding, while impulsivity, measured by anticipatory responding, was best controlled by olanzapine and haloperidol. Similar differences between typical and atypical antipsychotics were observed in a previous study, in which clozapine suppressed the CPP-induced accuracy deficits and anticipatory responding, while haloperidol had no effect on accuracy but prevented anticipatory and perseverative responding (Baviera et al. 2008). This confirms that the 5-CSRTT provides independent measures of different aspects of selective attention and inhibitory response control (Robbins 2002), which are underlined by distinct neural substrates (Chudasama and Muir 2001; Chudasama et al. 2003; Passetti et al. 2002) and can be dissociated at the level of receptor mechanisms (Carli et al. 2006).
The CPP-induced increase in omissions and latency to make a correct response might reflect changes in motor and/or motivational factors. However, it has been repeatedly shown that changes in motor activity and motivation are dissociated from changes in accuracy and response control (Carli and Samanin 1992; Mirjana et al. 2004; Robbins 2002).
Doses of aripiprazole preventing CPP-induced accuracy deficits in the 5-CSRTT also suppressed CPP’s effect on GLU release. Similarly, olanzapine dose-dependently reduced accuracy deficits and cortical GLU release. By contrast, 0.1 mg/kg haloperidol did not prevent the accuracy deficit and the rise of extracellular GLU induced by CPP, which was even enhanced. Although 0.3 mg/kg haloperidol reversed CPP’s effect on GLU (present study), this dose greatly increased omission errors (data not shown), so its effect in the 5-CSRTT could not be reliably assessed.
These findings suggest that activation of mechanisms suppressing GLU release in the mPFC may play a major role in the ability of aripiprazole and olanzapine to attenuate attention deficit induced by blockade of NMDA receptors and is consistent with our previous findings that drugs sharing the ability to prevent accuracy deficits in the 5-CSRTT suppressed CPP’s effects on GLU release in the rat mPFC (summarized in Table 1). It should be made clear that basal extracellular GLU in the mPFC as measured by microdialysis is mostly not neuronal (Melendez et al. 2005; Timmerman and Westerink 1997). By contrast, CPP-evoked GLU release was completely abolished by the sodium channel inhibitor tetrodotoxin (Ceglia et al. 2004), suggesting that it is attributable to increased action potential-dependent neuronal release.
Among the three antipsychotics examined, only olanzapine 1.0 mg/kg raised basal GLU release. However, the effect of olanzapine was far less than that of CPP. Although enhanced GLU release in the mPFC is associated with impaired performance in the 5-CSRTT, olanzapine by itself did not affect accuracy or other indices of attentional functioning. Higher doses of olanzapine greatly increased omissions and cannot be reliably tested in the 5-CSRTT (data not shown).
Preferential blockade of cortical inhibitory GABAergic interneurons, which, in turn, enhance cortical excitation by removing the inhibitory tone on pyramidal neurons likely underline the mechanism by which CPP increases GLU release (Homayoun and Moghaddam 2007b; Jackson et al. 2004). Consistently, CPP reduced extracellular GABA in the rat mPFC (Calcagno et al. 2009). In addition, blockade of NMDA receptors caused cortical activation in rodents (Gozzi et al. 2008; Homayoun and Moghaddam 2007b; Jackson et al. 2004; Suzuki et al. 2002), and these effects were prevented by the blockade of 5-HT2A receptors or stimulation of mGlu 2/3 receptors (Gozzi et al. 2010; Homayoun et al. 2005), which also prevented the release of GLU induced by NMDA receptor blockade (Ceglia et al. 2004; Moghaddam and Adams 1998). Furthermore, ketamine caused cortical activation in human volunteers (Breier et al. 1997; Vollenweider et al. 1997a), suggesting that NMDA receptors of the prefrontal cortex may be involved in mediating the cognitive impairment caused by this drug both in humans and rodents.
Although brain 5-HT has been consistently involved in the control of impulsivity, both depletion of brain 5-HT and elevated 5-HT release in the mPFC have been associated to impulsivity in the 5-CSRTT (Carli and Samanin 2000; Dalley et al. 2002; Harrison et al. 1997; Winstanley et al. 2004). In addition, endogenous 5-HT plays a major role in the control exerted by 5-HT2A receptors on CPP-induced GLU release (Calcagno et al. 2009) and the ability to suppress locomotor activity induced by dizocilpine (Martin et al. 1998). The fact that aripiprazole, olanzapine, and haloperidol suppressed the CPP-induced 5-HT release in the mPFC suggests that cortical 5-HT might contribute to the ability of these drugs to prevent the effects of CPP in the 5-CSRTT. However, no consistent relationship can be established between the ability of aripiprazole, olanzapine, haloperidol, or selective 5-HT agonists and antagonists to prevent CPP-induced impulsivity, perseverative responses, and accuracy deficits and changes in cortical 5-HT release (see Table 1).
The distinct, but partly overlapping, effects of aripiprazole, olanzapine, and haloperidol on attentional functioning and on different aspects of response control suggest that multiple mechanisms are involved. These were not addressed in the present study and we can only speculate on the mechanisms involved by drawing analogies with the effects of selective receptor agonists and antagonists. As summarized in Table 1, accuracy impairment induced by CPP in the 5-CSRTT is prevented by the stimulation of 5-HT1A and 5-HT2C receptors or the blockade of 5-HT2A receptors, while impulsivity is best controlled by the stimulation of 5-HT2C and 5-HT1A receptors or blockade of D2 receptor. Finally, compulsivity is prevented by blockade of D2 receptors or stimulation of 5-HT1A receptors. However, we cannot exclude that other mechanisms are involved in the action of the antipsychotics investigated in the present study, which act on other receptors in addition to those mentioned above (Bymaster et al. 1999; Schotte et al. 1996).
Aripiprazole is a potent 5-HT1A receptor partial agonist (DeLeon et al. 2004; Jordan et al. 2002a, b). It suppressed the firing rate of 5-HT neurons in the rat dorsal raphé (Bortolozzi et al. 2007; Stark et al. 2007) and ameliorated PCP-induced impairment in recognition memory and social behavior (Bruins Slot et al. 2005; Nagai et al. 2009; Snigdha and Neill 2008); the 5-HT1A receptor antagonist WAY100635 prevented these effects. A pattern of effects in the 5-CSRTT similar to those seen here with aripiprazole was observed after intracortical injection of 8-OH-DPAT (Carli et al. 2006), which also suppressed the CPP-induced rise of extracellular GLU (Calcagno et al. 2006). In addition, aripiprazole suppressed GLU release induced by the potassium channel blocker 4-aminopyridine in synaptosomes of the rat mPFC, and WAY100635 abolished this effect (Yang and Wang 2008).
5-HT2A receptors blockade may play a major role in olanzapine’s ability to prevent accuracy impairment and impulsivity, and CPP-induced GLU release as selective blockade of 5-HT2A receptors is sufficient to abolish these effects (Ceglia et al. 2004; Mirjana et al. 2004). Consistently, doses of olanzapine used in the present study occupy most 5-HT2A receptors in the rat frontal cortex (Knauer et al. 2008; Schotte et al. 1996) and completely suppressed the 5-HT2A receptor-mediated discriminative stimulus induced by 1-[2,5-dimethoxy-4-iodophenyl]-2-aminopropane (DOI; Sanchez and Arnt 2000). However, it is unlikely that 5-HT2A receptors are involved in aripiprazole’s effect, because significant in vivo occupation of these sites is attained only after 20 mg/kg or more (Natesan et al. 2006), which is well above the doses used in the present study. Poor in vivo occupancy of 5-HT2A receptors probably accounts for aripiprazole’s nonsignificant effect on the CPP-induced rise of anticipatory responding and the failure to prevent head twitches induced by 5-methoxy-N,N-dimethyl-tryptamine in mice (Hirose et al. 2004), two effects blocked by selective 5-HT2A receptor antagonists (Mirjana et al. 2004; Schreiber et al. 1995; Vickers et al. 2001).
Aripiprazole and olanzapine potently bind D2 receptors in vitro and in vivo (Natesan et al. 2006; Schotte et al. 1996; Zhang and Bymaster 1999) and suppress apomorphine-induced hypermotility with similar potency (Kikuchi et al. 1995; Morimoto et al. 2002). At 0.1 mg/kg, haloperidol, which occupies most brain D2 receptors (Mukherjee et al. 2001), did not prevent accuracy deficits and cortical GLU release induced by CPP but abolished anticipatory and perseverative over-responding. Thus, it is unlikely that D2 receptor blockade contributes to the ability of aripiprazole and olanzapine to reverse accuracy deficits and GLU release, but might play a role in the effects of aripiprazole, olanzapine, and haloperidol on response inhibition.
The suppression of CPP-induced 5-HT release by aripiprazole and olanzapine is consistent with their action on 5-HT1A and 5-HT2A receptors, respectively (see above), as stimulation of 5-HT1A or blockade of 5-HT2A receptors prevented CPP’s effects on 5-HT release (Calcagno et al. 2006; Ceglia et al. 2004). CPP-induced 5-HT release was suppressed by haloperidol, which also reduced basal 5-HT release, albeit only at the lowest dose. Similarly, only low doses of haloperidol suppressed basal 5-HT release in the striatum (Lucas et al. 2001). Thus, the involvement of D2 receptors in aripiprazole’s and olanzapine’s effects on 5-HT cannot be excluded.
Aripiprazole and/or olanzapine have moderate to high affinity for other receptors, including dopamine D1, D3, and D4, 5-HT2C, α1-adrenergic, histamine H1, and cholinergic M1 receptors (Bymaster et al. 1996; DeLeon et al. 2004), some of which modulate attention and GLU release under basal conditions or in response to NMDA receptor blockade (Lopez-Gil et al. 2009; Robbins 2002). Thus, it cannot be excluded that an action on one of these receptors or a concomitant effect on several of them contributes to the ability of these drugs to prevent attention deficits and cortical GLU release.
The rise of extracellular 5-HT in response to 3.0 mg/kg aripiprazole is surprising as previous studies found no effect in the mouse mPFC (Zocchi et al. 2005) and rat hippocampus (Assie et al. 2008) and a decrease in the rat and mouse mPFC (Bortolozzi et al. 2007). Increased extracellular 5-HT would be compatible with an action on 5-HT reuptake which is inhibited by aripiprazole with a Ki of 98 nM (Stark et al. 2007), a brain concentration probably achieved after 3.0 mg/kg aripiprazole (Shimokawa et al. 2005). The inclusion of a 5-HT reuptake inhibitor in the perfusion medium in one of the previous studies may well have precluded aripiprazole’s interaction with the 5-HT transporter favoring mechanisms such as the stimulation of 5-HT1A receptors leading to the inhibition of 5-HT release (Bortolozzi et al. 2007).
One possible limit to the relationship between GLU release and attention performance is that the modalities of CPP administration in behavioral and microdialysis experiments were quite different, a bolus injection of 50 ng/μl in the mPFC and a continuous infusion of 100 μM CPP through the probe. However, the delivery of 50 ng/μl CPP through a side cannula glued to the probe and perfusion of 100 μM CPP through the probe increased extracellular GLU to a similar extent (Calcagno et al. 2009). Thus, it is very likely that comparable doses of CPP were administered under both conditions. This strengthens the link between microdialysis and behavioral data.
In summary, the present findings show that the cognitive effects of antipsychotics may differ on the basis of their ability to reverse deficits in different aspects of attentional performance in the 5-CSRTT. The data also confirm that excessive GLU release in the mPFC is associated with attention deficits and is consistent with the suggestion that mPFC activity may be a substrate for the improved efficacy of clozapine in schizophrenia (Homayoun and Moghaddam 2007a). Aripiprazole and olanzapine, but not haloperidol, fully prevented some aspects of attention deficit in the 5-CSRTT and prevented GLU release induced by CPP. Both drugs show small but significant improvements in general cognitive functioning in schizophrenic patients, while neither drug was effective in improving executive functioning or sustained attention (Kern et al. 2006). In addition, it is debated whether there is any real differences in the ability of typical and atypical antipsychotics in improving cognitive functions in schizophrenic patients (Green et al. 2002; Keefe et al. 2004, 2007). Thus, it remains to be established whether selective suppression of GLU release might be one target for the development of novel antipsychotic drugs with enhanced effect on some aspects of cognitive deficits. Interestingly, the stimulation of mGlu2/3 receptors, which serve as autoreceptors at GLU synapses (Shigemoto et al. 1997), prevents NMDA receptor antagonist-evoked GLU release in the mPFC and deficits in attentional performance and working memory (Greco et al. 2005; Moghaddam et al. 1997; Moghaddam and Adams 1998) and holds potential for the treatment of schizophrenia (Patil et al. 2007).
References
Aghajanian GK, Marek GJ (1997) Serotonin induces excitatory postsynaptic potentials in apical dendrites of neocortical pyramidal cells. Neuropharmacology 36:589–599
Aghajanian GK, Marek GJ (1999) Serotonin, via 5-HT2A receptors, increases EPSCs in layer V pyramidal cells of prefrontal cortex by an asynchronous mode of glutamate release. Brain Res 825:161–171
Aghajanian GK, Marek GJ (2000) Serotonin model of schizophrenia: emerging role of glutamate mechanisms. Brain Res Brain Res Rev 31:302–312
Amargos-Bosch M, Bortolozzi A, Puig MV, Serrats J, Adell A, Celada P, Toth M, Mengod G, Artigas F (2004) Co-expression and in vivo interaction of serotonin1A and serotonin2A receptors in pyramidal neurons of prefrontal cortex. Cereb Cortex 14:281–299
Amargos-Bosch M, Artigas F, Adell A (2005) Effects of acute olanzapine after sustained fluoxetine on extracellular monoamine levels in the rat medial prefrontal cortex. Eur J Pharmacol 516:235–238
Amitai N, Semenova S, Markou A (2007) Cognitive-disruptive effects of the psychotomimetic phencyclidine and attenuation by atypical antipsychotic medications in rats. Psychopharmacology (Berl) 193:521–537
Assie MB, Carilla-Durand E, Bardin L, Maraval M, Aliaga M, Malfetes N, Barbara M, Newman-Tancredi A (2008) The antipsychotics clozapine and olanzapine increase plasma glucose and corticosterone levels in rats: comparison with aripiprazole, ziprasidone, bifeprunox and F15063. Eur J Pharmacol 592:160–166
Bakshi VP, Swerdlow NR, Geyer MA (1994) Clozapine antagonizes phencyclidine-induced deficits in sensorimotor gating of the startle response. J Pharmacol Exp Ther 271:787–794
Baviera M, Invernizzi RW, Carli M (2008) Haloperidol and clozapine have dissociable effects in a model of attentional performance deficits induced by blockade of NMDA receptors in the mPFC. Psychopharmacology (Berl) 196:269–280
Bortolozzi A, Diaz-Mataix L, Toth M, Celada P, Artigas F (2007) In vivo actions of aripiprazole on serotonergic and dopaminergic systems in rodent brain. Psychopharmacology (Berl) 191:745–758
Breier A, Malhotra AK, Pinals DA, Weisenfeld NI, Pickar D (1997) Association of ketamine-induced psychosis with focal activation of the prefrontal cortex in healthy volunteers. Am J Psychiatry 154:805–811
Bruins Slot LA, Kleven MS, Newman-Tancredi A (2005) Effects of novel antipsychotics with mixed D(2) antagonist/5-HT(1A) agonist properties on PCP-induced social interaction deficits in the rat. Neuropharmacology 49:996–1006
Burris KD, Molski TF, Xu C, Ryan E, Tottori K, Kikuchi T, Yocca FD, Molinoff PB (2002) Aripiprazole, a novel antipsychotic, is a high-affinity partial agonist at human dopamine D2 receptors. J Pharmacol Exp Ther 302:381–389
Bymaster FP, Calligaro DO, Falcone JF, Marsh RD, Moore NA, Tye NC, Seeman P, Wong DT (1996) Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology 14:87–96
Bymaster FP, Nelson DL, DeLapp NW, Falcone JF, Eckols K, Truex LL, Foreman MM, Lucaites VL, Calligaro DO (1999) Antagonism by olanzapine of dopamine D1, serotonin2, muscarinic, histamine H1 and alpha 1-adrenergic receptors in vitro. Schizophr Res 37:107–122
Calcagno E, Carli M, Invernizzi RW (2006) The 5-HT(1A) receptor agonist 8-OH-DPAT prevents prefrontocortical glutamate and serotonin release in response to blockade of cortical NMDA receptors. J Neurochem 96:853–860
Calcagno E, Carli M, Baviera M, Invernizzi RW (2009) Endogenous serotonin and serotonin2C receptors are involved in the ability of M100907 to suppress cortical glutamate release induced by NMDA receptor blockade. J Neurochem 108:521–532
Carli M, Samanin R (1992) 8-Hydroxy-2-(di-n-propylamino) tetralin impairs spatial learning in a water maze: role of postsynaptic 5-HT1A receptors. Br J Pharmacol 105:720–726
Carli M, Samanin R (2000) The 5-HT1A receptor agonist 8-OH-DPAT reduces rats’ accuracy of attentional performance and enhances impulsive responding in a five-choice serial reaction time task: role of presynaptic 5-HT1A receptors. Psychopharmacology 149:259–268
Carli M, Robbins TW, Evenden JL, Everitt BJ (1983) Effects of lesions to ascending noradrenergic neurones on performance of a 5-choice serial reaction task in rats; implications for theories of dorsal noradrenergic bundle function based on selective attention and arousal. Behav Brain Res 9:361–380
Carli M, Baviera M, Invernizzi RW, Balducci C (2006) Dissociable contribution of 5-HT1A and 5-HT2A receptors in the medial prefrontal cortex to different aspects of executive control such as impulsivity and compulsive perseveration in rats. Neuropsychopharmacology 31:757–767
Ceglia I, Carli M, Baviera M, Renoldi G, Calcagno E, Invernizzi RW (2004) The 5-HT receptor antagonist M100, 907 prevents extracellular glutamate rising in response to NMDA receptor blockade in the mPFC. J Neurochem 91:189–199
Chudasama Y, Muir JL (2001) Visual attention in the rat: a role for the prelimbic cortex and thalamic nuclei? Behav Neurosci 115:417–428
Chudasama Y, Passetti F, Rhodes SE, Lopian D, Desai A, Robbins TW (2003) Dissociable aspects of performance on the 5-choice serial reaction time task following lesions of the dorsal anterior cingulate, infralimbic and orbitofrontal cortex in the rat: differential effects on selectivity, impulsivity and compulsivity. Behav Brain Res 146:105–119
Dalley JW, Theobald DE, Eagle DM, Passetti F, Robbins TW (2002) Deficits in impulse control associated with tonically-elevated serotonergic function in rat prefrontal cortex. Neuropsychopharmacology 26:716–728
DeLeon A, Patel NC, Crismon ML (2004) Aripiprazole: a comprehensive review of its pharmacology, clinical efficacy, and tolerability. Clin Ther 26:649–666
Gozzi A, Large CH, Schwarz A, Bertani S, Crestan V, Bifone A (2008) Differential effects of antipsychotic and glutamatergic agents on the phMRI response to phencyclidine. Neuropsychopharmacology 33:1690–1703
Gozzi A, Crestan V, Turrini G, Clemens M, Bifone A (2010) Antagonism at serotonin 5-HT(2A) receptors modulates functional activity of frontohippocampal circuit. Psychopharmacology (Berl) 209:37–50
Greco B, Invernizzi RW, Carli M (2005) Phencyclidine-induced impairment in attention and response control depends on the background genotype of mice: reversal by the mGLU(2/3) receptor agonist LY379268. Psychopharmacology (Berl) 179:68–76
Green MF, Marder SR, Glynn SM, McGurk SR, Wirshing WC, Wirshing DA, Liberman RP, Mintz J (2002) The neurocognitive effects of low-dose haloperidol: a 2-year comparison with risperidone. Biol Psychiatry 51:972–978
Harrison AA, Everitt BJ, Robbins TW (1997) Central 5-HT depletion enhances impulsive responding without affecting the accuracy of attentional performance: interactions with dopaminergic mechanisms. Psychopharmacology (Berl) 133:329–342
Harvey PD, Keefe RS (2001) Studies of cognitive change in patients with schizophrenia following novel antipsychotic treatment. Am J Psychiatry 158:176–184
Higgins GA, Enderlin M, Homan M, Fletcher PJ (2003) The 5-HT2A receptor antagonist M100,907 attenuates motor and “impulsive-type” behaviours produced by NMDA receptor antagonism. Psychopharmacology 170:309–319
Hirose T, Uwahodo Y, Yamada S, Miwa T, Kikuchi T, Kitagawa H, Burris KD, Altar CA, Nabeshima T (2004) Mechanism of action of aripiprazole predicts clinical efficacy and a favourable side-effect profile. J Psychopharmacol 18:375–383
Hoffman DC, Donovan H, Cassella JV (1993) The effects of haloperidol and clozapine on the disruption of sensorimotor gating induced by the noncompetitive glutamate antagonist MK-801. Psychopharmacology (Berl) 111:339–344
Holcomb HH, Lahti AC, Medoff DR, Cullen T, Tamminga CA (2005) Effects of noncompetitive NMDA receptor blockade on anterior cingulate cerebral blood flow in volunteers with schizophrenia. Neuropsychopharmacology 30:2275–2282
Homayoun H, Moghaddam B (2007a) Fine-tuning of awake prefrontal cortex neurons by clozapine: comparison with haloperidol and N-desmethylclozapine. Biol Psychiatry 61:679–687
Homayoun H, Moghaddam B (2007b) NMDA receptor hypofunction produces opposite effects on prefrontal cortex interneurons and pyramidal neurons. J Neurosci 27:11496–11500
Homayoun H, Jackson ME, Moghaddam B (2005) Activation of metabotropic glutamate 2/3 receptors reverses the effects of NMDA receptor hypofunction on prefrontal cortex unit activity in awake rats. J Neurophysiol 93:1989–2001
Jackson ME, Homayoun H, Moghaddam B (2004) NMDA receptor hypofunction produces concomitant firing rate potentiation and burst activity reduction in the prefrontal cortex. Proc Natl Acad Sci USA 101:8467–8472
Javitt DC, Zukin SR (1991) Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry 148:1301–1308
Jordan S, Chen R, Johnson J, Regardie K, Tadori Y, Kikuchi T (2002a) Aripiprazole is a potent, partial agonist at cloned human D2L and native 5-HT1A receptors. Eur Neuropsychopharmacol 13:S293
Jordan S, Koprivica V, Chen R, Tottori K, Kikuchi T, Altar CA (2002b) The antipsychotic aripiprazole is a potent, partial agonist at the human 5-HT1A receptor. Eur J Pharmacol 441:137–140
Keefe RS, Silva SG, Perkins DO, Lieberman JA (1999) The effects of atypical antipsychotic drugs on neurocognitive impairment in schizophrenia: a review and meta-analysis. Schizophr Bull 25:201–222
Keefe RS, Seidman LJ, Christensen BK, Hamer RM, Sharma T, Sitskoorn MM, Lewine RR, Yurgelun-Todd DA, Gur RC, Tohen M, Tollefson GD, Sanger TM, Lieberman JA (2004) Comparative effect of atypical and conventional antipsychotic drugs on neurocognition in first-episode psychosis: a randomized, double-blind trial of olanzapine versus low doses of haloperidol. Am J Psychiatry 161:985–995
Keefe RS, Bilder RM, Davis SM, Harvey PD, Palmer BW, Gold JM, Meltzer HY, Green MF, Capuano G, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, Davis CE, Hsiao JK, Lieberman JA (2007) Neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE Trial. Arch Gen Psychiatry 64:633–647
Kern RS, Green MF, Cornblatt BA, Owen JR, McQuade RD, Carson WH, Ali M, Marcus R (2006) The neurocognitive effects of aripiprazole: an open-label comparison with olanzapine. Psychopharmacology (Berl) 187:312–320
Kikuchi T, Tottori K, Uwahodo Y, Hirose T, Miwa T, Oshiro Y, Morita S (1995) 7-(4-[4-(2, 3-Dichlorophenyl)-1-piperazinyl]butyloxy)-3, 4-dihydro-2(1H)-quinolinone (OPC-14597), a new putative antipsychotic drug with both presynaptic dopamine autoreceptor agonistic activity and postsynaptic D2 receptor antagonistic activity. J Pharmacol Exp Ther 274:329–336
Knauer CS, Campbell JE, Galvan B, Bowman C, Osgood S, Buist S, Buchholz L, Henry B, Wong EH, Shahid M, Grimwood S (2008) Validation of a rat in vivo [(3)H]M100907 binding assay to determine a translatable measure of 5-HT(2A) receptor occupancy. Eur J Pharmacol 591:136–141
Lopez-Gil X, Artigas F, Adell A (2009) Role of different monoamine receptors controlling MK-801-induced release of serotonin and glutamate in the medial prefrontal cortex: relevance for antipsychotic action. Int J Neuropsychopharmacol 12:487–499
Lucas G, Di Matteo V, De Deurwaerdere P, Porras G, Martin-Ruiz R, Artigas F, Esposito E, Spampinato U (2001) Neurochemical and electrophysiological evidence that 5-HT4 receptors exert a state-dependent facilitatory control in vivo on nigrostriatal, but not mesoaccumbal, dopaminergic function. Eur J Neurosci 13:889–898
Martin P, Waters N, Schmidt CJ, Carlsson A, Carlsson ML (1998) Rodent data and general hypothesis: antipsychotic action exerted through 5-HT2A receptor antagonism is dependent on increased serotonergic tone. J Neural Transm 105:365–396
Melendez RI, Vuthiganon J, Kalivas PW (2005) Regulation of extracellular glutamate in the prefrontal cortex: focus on the cystine glutamate exchanger and group I metabotropic glutamate receptors. J Pharmacol Exp Ther 314:139–147
Meltzer HY, McGurk SR (1999) The effects of clozapine, risperidone, and olanzapine on cognitive function in schizophrenia. Schizophr Bull 25:233–255
Mirjana C, Baviera M, Invernizzi RW, Balducci C (2004) The serotonin 5-HT2A receptors antagonist M100907 prevents impairment in attentional performance by NMDA receptor blockade in the rat prefrontal cortex. Neuropsychopharmacology 29:1637–1647
Miyamoto Y, Yamada K, Noda Y, Mori H, Mishina M, Nabeshima T (2001) Hyperfunction of dopaminergic and serotonergic neuronal systems in mice lacking the NMDA receptor epsilon1 subunit. J Neurosci 21:750–757
Moghaddam B, Adams BW (1998) Reversal of phencyclidine effects by a group II metabotropic glutamate receptor agonist in rats. Science 281:1349–1352
Moghaddam B, Jackson ME (2003) Glutamatergic animal models of schizophrenia. Ann NY Acad Sci 1003:131–137
Moghaddam B, Adams B, Verma A, Daly D (1997) Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. J Neurosci 17:2921–2927
Morimoto T, Hashimoto K, Yasumatsu H, Tanaka H, Fujimura M, Kuriyama M, Kimura K, Takehara S, Yamagami K (2002) Neuropharmacological profile of a novel potential atypical antipsychotic drug Y-931 (8-fluoro-12-(4-methylpiperazin-1-yl)-6H-[1]benzothieno[2, 3-b][1, 5] benzodiazepine maleate). Neuropsychopharmacology 26:456–467
Mukherjee J, Christian BT, Narayanan TK, Shi B, Mantil J (2001) Evaluation of dopamine D-2 receptor occupancy by clozapine, risperidone, and haloperidol in vivo in the rodent and nonhuman primate brain using 18F-fallypride. Neuropsychopharmacology 25:476–488
Nagai T, Murai R, Matsui K, Kamei H, Noda Y, Furukawa H, Nabeshima T (2009) Aripiprazole ameliorates phencyclidine-induced impairment of recognition memory through dopamine D1 and serotonin 5-HT1A receptors. Psychopharmacology (Berl) 202:315–328
Natesan S, Reckless GE, Nobrega JN, Fletcher PJ, Kapur S (2006) Dissociation between in vivo occupancy and functional antagonism of dopamine D2 receptors: comparing aripiprazole to other antipsychotics in animal models. Neuropsychopharmacology 31:1854–1863
Passetti F, Chudasama Y, Robbins TW (2002) The frontal cortex of the rat and visual attentional performance: dissociable functions of distinct medial prefrontal subregions. Cereb Cortex 12:1254–1268
Patil ST, Zhang L, Martenyi F, Lowe SL, Jackson KA, Andreev BV, Avedisova AS, Bardenstein LM, Gurovich IY, Morozova MA, Mosolov SN, Neznanov NG, Reznik AM, Smulevich AB, Tochilov VA, Johnson BG, Monn JA, Schoepp DD (2007) Activation of mGlu2/3 receptors as a new approach to treat schizophrenia: a randomized phase 2 clinical trial. Nat Med 13:1102–1107
Paxinos G, Watson C (1986) The rat brain in stereotaxic coordinates. Academic Press
Robbins TW (2002) The 5-choice serial reaction time task: behavioural pharmacology and functional neurochemistry. Psychopharmacology (Berl) 163:362–380
Robinson TE, Whishaw IQ (1988) Normalization of extracellular dopamine in striatum following recovery from a partial unilateral 6-OHDA lesion of the substantia nigra: a microdialysis study in freely moving rats. Brain Res 450:209–224
Rodefer JS, Nguyen TN, Karlsson JJ, Arnt J (2008) Reversal of subchronic PCP-induced deficits in attentional set shifting in rats by sertindole and a 5-HT6 receptor antagonist: comparison among antipsychotics. Neuropsychopharmacology 33:2657–2666
Sanchez C, Arnt J (2000) In-vivo assessment of 5-HT2A and 5-HT2C antagonistic properties of newer antipsychotics. Behav Pharmacol 11:291–298
Schotte A, Janssen PF, Gommeren W, Luyten WH, Van Gompel P, Lesage AS, De Loore K, Leysen JE (1996) Risperidone compared with new and reference antipsychotic drugs: in vitro and in vivo receptor binding. Psychopharmacology (Berl) 124:57–73
Schreiber R, Brocco M, Audinot V, Gobert A, Veiga S, Millan MJ (1995) (1-(2, 5-dimethoxy-4 iodophenyl)-2-aminopropane)-induced head-twitches in the rat are mediated by 5-hydroxytryptamine (5-HT) 2A receptors: modulation by novel 5-HT2A/2C antagonists, D1 antagonists and 5-HT1A agonists. J Pharmacol Exp Ther 273:101–112
Scruggs JL, Patel S, Bubser M, Deutch AY (2000) DOI-induced activation of the cortex: dependence on 5-HT2A heteroceptors on thalamocortical glutamatergic neurons. J Neurosci 20:8846–8852
Scruggs JL, Schmidt D, Deutch AY (2003) The hallucinogen 1-[2, 5-dimethoxy-4-iodophenyl]-2-aminopropane (DOI) increases cortical extracellular glutamate levels in rats. Neurosci Lett 346:137–140
Shigemoto R, Kinoshita A, Wada E, Nomura S, Ohishi H, Takada M, Flor PJ, Neki A, Abe T, Nakanishi S, Mizuno N (1997) Differential presynaptic localization of metabotropic glutamate receptor subtypes in the rat hippocampus. J Neurosci 17:7503–7522
Shimokawa Y, Akiyama H, Kashiyama E, Koga T, Miyamoto G (2005) High performance liquid chromatographic methods for the determination of aripiprazole with ultraviolet detection in rat plasma and brain: application to the pharmacokinetic study. J Chromatogr B Analyt Technol Biomed Life Sci 821:8–14
Snigdha S, Neill JC (2008) Improvement of phencyclidine-induced social behaviour deficits in rats: involvement of 5-HT1A receptors. Behav Brain Res 191:26–31
Stark AD, Jordan S, Allers KA, Bertekap RL, Chen R, Mistry Kannan T, Molski TF, Yocca FD, Sharp T, Kikuchi T, Burris KD (2007) Interaction of the novel antipsychotic aripiprazole with 5-HT1A and 5-HT 2A receptors: functional receptor-binding and in vivo electrophysiological studies. Psychopharmacology (Berl) 190:373–382
Suzuki Y, Jodo E, Takeuchi S, Niwa S, Kayama Y (2002) Acute administration of phencyclidine induces tonic activation of medial prefrontal cortex neurons in freely moving rats. Neuroscience 114:769–779
Timmerman W, Westerink BH (1997) Brain microdialysis of GABA and glutamate: what does it signify? Synapse 27:242–261
Vickers SP, Easton N, Malcolm CS, Allen NH, Porter RH, Bickerdike MJ, Kennett GA (2001) Modulation of 5-HT(2A) receptor-mediated head-twitch behaviour in the rat by 5-HT(2C) receptor agonists. Pharmacol Biochem Behav 69:643–652
Vollenweider FX, Leenders KL, Oye I, Hell D, Angst J (1997a) Differential psychopathology and patterns of cerebral glucose utilisation produced by (S)- and (R)-ketamine in healthy volunteers using positron emission tomography (PET). Eur Neuropsychopharmacol 7:25–38
Vollenweider FX, Leenders KL, Scharfetter C, Antonini A, Maguire P, Missimer J, Angst J (1997b) Metabolic hyperfrontality and psychopathology in the ketamine model of psychosis using positron emission tomography (PET) and [18F]fluorodeoxyglucose (FDG). Eur Neuropsychopharmacol 7:9–24
Winstanley CA, Dalley JW, Theobald DE, Robbins TW (2004) Fractionating impulsivity: contrasting effects of central 5-HT depletion on different measures of impulsive behavior. Neuropsychopharmacology 29:1331–1343
Yang TT, Wang SJ (2008) Aripiprazole and its human metabolite OPC14857 reduce, through a presynaptic mechanism, glutamate release in rat prefrontal cortex: possible relevance to neuroprotective interventions in schizophrenia. Synapse 62:804–818
Zhang W, Bymaster FP (1999) The in vivo effects of olanzapine and other antipsychotic agents on receptor occupancy and antagonism of dopamine D1, D2, D3, 5HT2A and muscarinic receptors. Psychopharmacology (Berl) 141:267–278
Zhou FM, Hablitz JJ (1999) Activation of serotonin receptors modulates synaptic transmission in rat cerebral cortex. J Neurophysiol 82:2989–2999
Zocchi A, Fabbri D, Heidbreder CA (2005) Aripiprazole increases dopamine but not noradrenaline and serotonin levels in the mouse prefrontal cortex. Neurosci Lett 387:157–161
Acknowledgment
This work was supported by a research grant from Brystol-Myers Squibb (Italy). Olanzapine was kindly donated by Eli-Lilly and Company (USA). We are grateful to JD Baggott for language editing. The authors have nothing to disclose.
Conflicts of Interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carli, M., Calcagno, E., Mainolfi, P. et al. Effects of aripiprazole, olanzapine, and haloperidol in a model of cognitive deficit of schizophrenia in rats: relationship with glutamate release in the medial prefrontal cortex. Psychopharmacology 214, 639–652 (2011). https://doi.org/10.1007/s00213-010-2065-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-010-2065-7