Abstract
The main objective of the present study was to establish whether the mixed σ1/muscarinic ligand ANAVEX2-73, shown to be neuroprotective in Alzheimer’s disease (AD) models in vivo and currently in clinical phase I/IIa, could have the ability to reduce the appearance of hyperphosphorylated Tau and amyloid-β1–42 (Aβ1–42) in the Aβ25–35 mouse model of AD. We therefore first confirmed that Aβ25–35 injection induced hyperphosphorylation of Tau protein, by showing that it rapidly decreased Akt activity and activated glycogen synthase kinase-3β (GSK-3β) in the mouse hippocampus. Second, we showed that the kinase activation, and resulting Tau alteration, directly contributed to the amyloid toxicity, as co-administration of the selective GSK-3β inhibitor 2-thio(3-iodobenzyl)-5-(1-pyridyl)-[1,3,4]-oxidiazole blocked both Tau phosphorylation and Aβ25–35-induced memory impairments. Third, we analyzed the ANAVEX2-73 effect on Tau phosphorylation and activation of the related kinase pathways (Akt and GSK-3β). And fourth, we also addressed the impact of the drug on Aβ25–35-induced Aβ1–42 seeding and observed that the compound significantly blocked the increase in Aβ1–42 and C99 levels in the hippocampus, suggesting that it may alleviate amyloid load in AD models. The comparison with PRE-084, a selective and reference σ1 receptor agonist, and xanomeline, a muscarinic ligand presenting similar profile as ANAVEX2-73 on M1 and M2 subtypes, confirmed that both muscarinic and σ1 targets are involved in the ANAVEX2-73 effects. The drug, acting synergistically on both targets, but with moderate affinity, presents a promising pharmacological profile.
Similar content being viewed by others
INTRODUCTION
Alzheimer’s disease (AD) is the most prevalent and devastating neurodegenerative dementia (Villard et al, 2011). The two physiopathological hallmarks are extracellular deposition of amyloid-β (Aβ) proteins, under the form of oligomers and plaques, and intracellular neurofibrillary tangles (NFTs). NFT are mainly constituted of hyper- and abnormally phosphorylated forms of the microtubule-associated Tau protein (Selkoe, 2004). Although the role of both Aβ and NFT in promoting neurotoxicity in the brain and related cognitive loss is highly recognized, the signalling pathways and underlying mechanisms are not yet clarified. It has been proposed that glycogen synthase kinase-3β (GSK-3β), a kinase with several roles in brain physiology, may be important as this is one of the major kinases responsible for Tau hyperphosphorylation (Kosik, 1992) and as it may be involved in Aβ-mediated toxicity in AD. Overactivation of GSK-3β in neurons is associated with cognitive impairments, Aβ production, neuronal death, and neuroinflammation (Bhat et al, 2004; Hooper et al, 2008). GSK-3β overactivation results in Tau hyperphosphorylation, microtubule disruption, and neuronal apoptosis (Kosik, 1992; Bhat et al, 2000, Hetman et al, 2000; Lucas et al, 2001; Beurel and Jope, 2006; DaRocha-Souto et al, 2012). Inhibition of GSK-3β activity also directly participates in synaptic plasticity and memory consolidation by allowing, for instance, a blockade of long-term depression following the induction of long-term potentiation (Peineau et al, 2007). Moreover, mice overexpressing GSK-3β showed impaired long-term potentiation and memory deficits (Hernandez et al, 2002), which could be attributable to impaired integration of Akt and Wnt signalling onto mammalian target of rapamycin (mTOR) stimulation (Ma et al, 2010, 2011). Aβ peptides also activate directly GSK-3β in vitro and in vivo, although the mechanism remains unclear (Kim et al, 2003; Akiyama et al, 2005; Klementiev et al, 2007; Zussy et al, 2011). Finally, GSK-3β could have a critical role in Aβ production (for review, see Cai et al, 2012). The kinase modulates APP processing and regulates Aβ production by interfering with APP cleavage at the γ-secretase complex level, as the APP and presenilin-1, a component of γ-secretase complex, are substrates of GSK-3β. It may also enhance β-secretase activity and downregulate α-secretase through protein kinase C (PKC) and ADAMs, other substrates of the kinase. GSK-3β inhibitors have therefore been proposed as neuroprotective drugs in AD, in preclinical assays, and clinical trials (Bhat et al, 2004; Hu et al, 2009).
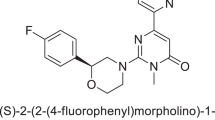
In search of new therapeutic drugs with potent neuroprotective ability in AD and not directly targeting amyloid or Tau proteins, we identified agonists of the σ1 chaperone protein (Meunier et al, 2006) and more particularly mixed muscarinic/σ1 ligands belonging to the ANAVEX series (Vamvakides, 2002a, 2002b). The σ1 protein is a chaperone of the endoplasmic reticulum (ER), preferentially located on membranes forming focal contacts between ER and mitochondria (Hayashi and Su, 2007). In basal conditions, the σ1 protein forms complex with other chaperones such as GRP78/BiP. Upon ER Ca2+ depletion or via ligand stimulation, the σ1 protein dissociates from BiP, leading to a prolonged Ca2+ signalling via inositol trisphosphate-1,4,5 receptors (Hayashi and Su, 2007). Under subsequent chronic ER stress, the σ1 protein can also translocate to reach plasma membrane (Morin-Surun et al, 1999), recruiting Ca2+-dependent intracellular cascades, including phospholipase C (PLC) and PKC (Morin-Surun et al, 1999; Monnet et al, 2003) and modifying the composition and functionality of the lipid-rich microdomains known as lipid rafts (Hayashi and Su, 2001, 2003). Increasing or activating σ1 proteins in cells counteracts ER stress response, whereas decreasing or inactivating them enhances apoptosis (Hayashi and Su, 2007). Modifying σ1 protein activation using effective agonists therefore mediates a unique pharmacological action on Ca2+ homeostasis and signal transduction pathways, with major impacts on cellular response and plasticity. The idea of developing mixed σ1/muscarinic ligands was therefore based on the capability to simultaneously activate a neuroprotective pathway, eg, the M1/PLC/PKC pathway, and amplify it, through a concomitant activation of the σ1 protein (Vamvakides, 2002a, 2002b; Espallergues et al, 2007; Villard et al, 2009, 2011). Tetrahydro-N,N-dimethyl-2,2-diphenyl-3-furanmethanamine hydrochloride (ANAVEX2-73) presents such a mixed σ1/muscarinic receptor profile, with a moderate affinity range. Indeed, the compound has a sub-micromolar affinity for the σ1 receptor (IC50=0.86 μM) and micromolar affinities for muscarinic human recombinant M1—M4 receptors (IC50=3.3–5.2 μM), sodium channel site 2 (IC50=5.1 μM), and N-methyl-D-aspartic acid receptors (IC50=8.0 μM; Vamvakides, 2002a, 2002b). The compound is a potent anti-amnesic drug, in mice treated with the muscarinic receptor antagonist scopolamine, the N-methyl-D-aspartic acid receptor antagonist dizocilpine, or Aβ25–35 peptide (Villard et al, 2011). The compound also showed, at sub-mg/kg intraperitoneal (i.p.) doses, a marked neuroprotective activity in vivo and prevented the oxidative stress, induction of caspases, cellular loss, and learning deficits observed 1 week after Aβ25–35 injection in mice (Villard et al, 2011).
The toxicity induced after such central injection of the Aβ25–35 fragment in oligomeric form in mice and rats was repeatedly shown to result in neuroinflammation and reactive gliosis, pro-apoptotic caspases activity, oxidative stress, reduction in the number of neurons measured in hippocampal pyramidal cell layers, loss of cholinergic neurons, and memory deficits (Maurice et al, 1996; Delobette et al, 1997; Stepanichev et al, 2003, 2004, 2006; Meunier et al, 2006; Klementiev et al, 2007; Chavant et al, 2010; Villard et al, 2009, 2011; Zussy et al, 2011). It is at present widely used to detect the neuroprotective potential of new drugs and natural derivatives (Ruan et al, 2010; Kim et al, 2011; Lu et al, 2012; Wang et al, 2012; Yang et al, 2012). Interestingly, the Aβ25–35 injection resulted not only in an aggressive amyloid toxicity but also in accumulation of endogenous Aβ species and Tau hyperphosphorylation, as observed in AD physiopathology. One week after Aβ25–35 injection, APP and Aβ1–42 levels were increased in the hippocampus and cortex, Aβ-expressing cells could be visualized using immunohistochemistry and β-secretase cleavage products, such as the C-terminal fragment C99, could be detected (Klementiev et al, 2007; Chavant et al, 2010; Zussy et al, 2011). Moreover, an increase in Tau phosphorylation on physiological or AD-related pathological epitopes induced by Aβ25–35 injection in mice was reported in several studies (Dudas et al, 2002; Klementiev et al, 2007; Deng et al, 2010). The model indeed appeared highly suitable to analyze the time course of kinase activations (Akt and GSK-3β) within days after Aβ injection and the resulting induction of Tau hyper- and abnormal phosphorylation.
Muscarinic ligands, and particularly M1 and M3 receptor agonists, have been shown to increase formation of sAPPα, preventing the formation of Aβ, and to target GSK-3β (for reviews, see Fisher, 2008, 2012). For instance, M1 receptor activation by AF267B resulted in elevation of PKC, extracellular signal-regulated protein kinase 1/2, ADAM17, and C83 fragment combined with decreased Aβ1–42, C99, GSK-3β activity, and Tau hyperphosphorylation (Fisher, 2012). AF267B also inhibited β-secretase (BACE1) expression in 3xTg-AD mice (Caccamo et al, 2006). In the present study, we took advantage of the Aβ25–35 model to analyze the ANAVEX2-73 effects on these parameters. However, as a pre-requisite to the study, we first analyzed the activity of Akt and GSK-3β after Aβ25–35 injection and, by using the selective GSK-3β inhibitor 2-thio(3-iodobenzyl)-5-(1-pyridyl)-[1,3,4]-oxidiazole (Tibpo), we showed that GSK-3β activation is a major component of the Aβ25–35-induced Tau phosphorylation, toxicity, and behavioral deficits. Second, we examined the potency of ANAVEX2-73 to restore Akt and GSK-3β activities and prevent Tau hyperphosphorylation, on one hand, and to attenuate Aβ1–42 generation on the other hand. Moreover, the selective muscarinic ligand xanomeline and σ1 agonist PRE-084 were examined in parallel to define the muscucarinic and σ1 components in the observed effects of ANAVEX2-73.
MATERIALS AND METHODS
Animals
Male Swiss OF-1 mice (Depré, St Doulchard, France) aged 7–9 weeks and weighing 32±2 g were used. They were housed in plastic cages in groups with free access to food and water, except during behavioral experiments. They were kept in a regulated environment (23±1 °C, 50–60% humidity) under a 12 h light/dark cycle (light on at 0800 hours). Behavioral experiments were carried out between 1000 and 1600 hours, in an experimental room within the animal facility. Mice were habituated 30 min before each experiment. All animal procedures were conducted in strict adherence to the EU Directive 86/609, modified by the decrees 87-848 and 2001-464.
Drugs and Administration Procedures
The amyloid-β[25–35] peptide (Aβ25–35) and scrambled Aβ25–35 peptide (Sc.Aβ) were purchased from Genepep (Saint-Jean-de-Védas, France). They were solubilized in sterile distilled water at a concentration of 3 mg/ml and stored at −20 °C until use. Before injection, peptides were incubated at 37 °C for 4 days, allowing Aβ25–35, but not Sc.Aβ, to form oligomers. They were administered intracerebroventricularly (i.c.v.) in a final volume of 3 μl per mouse, as previously described (Maurice et al, 1996, 1998; Meunier et al, 2006; Villard et al, 2009).
The GSK-3β inhibitor Tibpo was from Santa Cruz Biotechnology (GSK-3 Inhibitor II: sc-24020; Delaware, CA, USA; Naerum et al, 2002; Koh et al, 2005). It was solubilized in dimethylsulfoxide 40% and injected i.c.v. simultaneously with the amyloid peptide (final dimethylsulfoxide concentration 10%). Tetrahydro-N,N-dimethyl-2,2-diphenyl-3-furanmethanamine hydrochloride (ANAVEX2-73) was synthesized in the laboratory (Anavex Life Sciences). PRE-084 was a gift from Dr Tsung-Ping Su (Baltimore, MD, USA). Xanomeline was purchased from Sigma-Aldrich (St Quentin-Fallavier, France). Drugs were solubilized in physiological saline at the concentration of 5 mg/ml. They were then brought up to each dose by dilution and injected in a volume of 100 μl/20 g body weight. Animals were used between days 1 and 9 after i.c.v. injections for behavioral testing or killed before biochemical measures.
Spontaneous Alternation Performances
Each mouse, naive to the apparatus, was placed at the end of one arm in a Y-maze (three arms, 50 cm long, 60° separate) and allowed to move freely through the maze during a single 8-min session. The series of arm entries, including possible returns into the same arm, was recorded visually. An alternation was defined as entries into all three arms on consecutive trials. The number of the total possible alternations was therefore the total number of arm entries minus two and the percentage of alternation was calculated as (actual alternations/total possible alternations) × 100.
Step-through Passive Avoidance Test
The apparatus consisted of an illuminated compartment with white polyvinylchloride walls (15 × 20 × 15 cm3 high), a darkened compartment with black polyvinylchloride walls (15 × 20 × 15 cm3 high), and a grid floor. A guillotine door separated each compartment. A 60-W lamp positioned 40 cm above the apparatus lit the white compartment during the experimental period. Scrambled foot shocks (0.3 mA for 3 s) were delivered to the grid floor using a shock generator scrambler (Lafayette Instruments, Lafayette, MA, USA). The guillotine door was initially closed during the training session. Each mouse was placed into the white compartment. After 5 s, the door was raised. When the mouse entered the darkened compartment and placed all its paws on the grid floor, the door was gently closed and the scrambled foot shock was delivered for 3 s. The step-through latency, ie, the latency spent to enter the dark compartment, and the number of vocalizations was recorded. The number of vocalizations did not differ among groups, indicating that shock sensitivity was unaffected by the treatments (data not shown). The retention test was carried out 24 h after training. Each mouse was placed again into the white compartment. After 5 s, the door was raised. The step-through latency was recorded up to 300 s. Animals entered in the dark compartment or were placed into it and the escape latency, ie, the time spent to return into the white compartment, was also measured up to 300 s. The two parameters were measured although they do not rely on similar memory stimuli. The step-through latency involves reinforced stimuli and is the direct measure of passive avoidance behavior. The escape latency relies on a supplementary sensory information, the contact with the grid floor that per se activates specific retrieval pathways, but includes an interfering information: the absence of electric shock in this compartment during the retention session.
Novel Object Recognition Memory
Six days after peptide and drug injections, mice were placed individually in a squared open field (50 × 50 × 50 cm3 high) made in white Plexiglas with a floor equipped with infrared light-emitting diodes. On day 6 after peptide and drug injections, mice were habituated to the open field (session 1). During 10 min, the locomotor activity of the animals was captured through an IR-sensitive camera and analyzed using the Videotrack software (Viewpoint, Champagne-au-Mont-d’Or, France). The activity was analyzed in terms of total distance travelled (m), locomotor speed (cm/s), and percentage of presence in the 25 × 25 cm2 central area defined by the software. On day 7 after peptide and drug injections (session 2), two identical objects (50 ml plastic vials with caps) were placed at defined positions, at ¼ and ¾ of one diagonal of the open field. Each mouse was placed in the open field and the exploratory activity was recorded during 10 min. The activity was analyzed using the Nosetrack protocol (Viewpoint) in terms of number of contacts with objects and duration of the contacts. On day 8 after the injections (session 3), the object in position #2 was replaced by a novel one (a soft plastic chair feet protection) differing in color shape and texture from the familiar object. Each mouse was placed again in the open field and the exploratory activity recorded during 10 min. The activity was analyzed similarly. The preferential exploration index was calculated as the ratio of the number (or duration) of contacts with the object in position #2 over the total number (or duration) of contacts with the two objects. As the analyses in terms of number of contacts or duration of contacts led to strictly similar results (data not shown), only the analyses in terms of number of contacts are presented. Animals showing no contact with one object or less than 10 contacts with objects, during the session 2 or 3, were discarded from the study. It represented 32 animals over 376, ie, 8.5%, attrition in this procedure.
Lipid Peroxydation Measures
Mice were killed by decapitation and brains were rapidly removed, the hippocampus dissected out, weighed, and kept in liquid nitrogen until assayed. After thawing, the hippocampus was homogenized in cold methanol (1/10w/v), centrifuged at 1000 g during 5 min and the supernatant collected. Homogenate was added to a solution containing 1 mM FeSO4, 0.25 M H2SO4, 1 mM xylenol orange, and incubated for 30 min at room temperature. Absorbance was measured at 580 nm (A5801), and 10 μl of 1 mM cumene hydroperoxyde (CHP) was added to the sample and incubated for 30 min at room temperature, to determine the maximal oxidation level. Absorbance was measured at 580 nm (A5802). The level of lipid peroxydation was determined as CHP equivalents according to: CHP eq.=A5801/A5802 × [CHP (nmol)] × dilution, and expressed as CHP eq. per wet tissue weight.
Murine Aβ1–40/42 Contents Measured by ELISA
Mice were killed by decapitation 7 days after Aβ25–35 injection and brains were rapidly removed, the hippocampus dissected out, weighted, frozen in liquid nitrogen, and stored at −80 °C until assayed. After thawing, the hippocampus was homogenized in 50 mM Tris-150 mM NaCl buffer, pH 7.5, and sonicated for 20 s. After centrifugation (16 100 g for 15 min, 4 °C), supernatants were used for mouse Aβ1–40 ELISA assay (E90864Mu, Uscn Life Science, Euromedex, Souffelweyersheim, France) or for mouse Aβ1–42 ELISA assay (E90946Mu, Uscn Life Science), according to the manufacturer’s instructions. Absorbance was read at 450 nm and sample concentration was calculated using the standard curve. Results were then expressed in pg of Aβ1–40/42/mg of tissue.
Western Blotting
Mice were decapitated at indicated days after Aβ25–35 peptide injection. The hippocampus was removed on an ice-cold Petri dish and stored at −80 °C. Tissues were homogenized by sonication in a lysis buffer (125 mM Tris-HCl pH 6.8, 4% SDS, 20% glycerol) including a protease and phosphatase inhibitors cocktail (Roche Diagnostics, Meylan, France). Homogenates were heated at 70 °C for 10 min and centrifuged at 16 000 g for 30 min at 15 °C. Protein concentration was determined using the Pierce BCA assay (Pierce Biotechnology, Rockford, IL, USA) according to the manufacturer’s instructions.
Proteins, 20–50 μg per lane, were resolved on a 10% SDS-polyacrylamid gel, except for C99 determination where a 15% SDS-polyacrylamid gel was used. Proteins were then transferred to a PVDF membrane (GE Healthcare, Orsay, France). After 1 h blocking in 5% non-fat dry milk in a 20 mM Tris-buffered saline, pH=7.5, buffer containing 0.1% Tween-20 (TBS-T), membranes were incubated overnight at 4 °C with the primary antibodies (see Table 1). After brief washes, membranes were incubated for 1 h at room temperature with corresponding secondary antibody (Table 1). The immunoreactive bands were visualized with the enhanced chemiluminescence reagent (ECL, Pierce Biotechnology) using a Lumi-Imager F1 Workstation (Roche Diagnostic). Then, membranes were stripped using the Restore Western Blot Stripping Buffer (Pierce Biotechnology) and incubated with anti-GSK-3β, anti-Tau, anti-Akt, or anti-β-tubulin antibody (see Table 1). The intensity of peroxydase activity was quantified using the ImageJ software (NIH, Bethesda, MD, USA).
Statistical Analyses
Alternation percentages and biochemical data were expressed as mean±SEM. They were analyzed using one-way ANOVA (F values), followed by the Dunnett’s post-hoc multiple comparison test. Passive avoidance latencies were expressed as median and inter-quartile range, as an upper cutoff time was set. They were analyzed using a Kruskal–Wallis non-parametric ANOVA (H values), followed by the Dunn’s multiple comparisons test. Novel object contact preferences were analyzed using a one-sample t-test vs the no-preference level (50%). For reading clarity, ANOVA data were all reported in the figure legends. The level of statistical significance was p<0.05.
RESULTS
Time Course for Akt and GSK-3β Kinase Activation after Aβ25–35 Injection in Mice
As schematized in Figure 1a, Tau hyperphosphorylation in the brain is mainly due to a decrease in Akt activity, which inactivates GSK-3β by phosphorylating the kinase on an inactivating epitope, Ser9. In parallel, an increase in the kinase phosphorylation on an activating site, Tyr216, putatively regulated by PYK2 activity, also contributes to GSK-3β activation and to the hyperphosphorylation of Tau (Figure 1a). We therefore analyzed by western blot, the time course of Akt activation, by measuring the phospho (Ser473)Akt/total Akt ratio, and GSK-3β activation by measuring both the P(Ser9)GSK-3β/GSK-3β and P(Tyr216)GSK-3β/GSK-3β ratios.
Time course of phosphorylation of Akt and GSK-3β in the hippocampus of mice treated with Aβ25–35 peptide. (a) Signalling pathways involved, (b) P(S473)Akt/total Akt ratio, (c) P(S9)GSK-3β/total GSK-3β ratio, (d) P(Y216)GSK-3β/total GSK-3β ratio. PI3K, phospho-inositide 3-kinase; PDK1/2, protein kinase B; PYK2, proline-rich tyrosine kinase 2; Akt, serine/threonine protein kinase; GSK-3β, glycogen synthase kinase-3β. Typical blots are shown above the graphs. Lanes were from the same blot but placed in the same treatment order as shown for the graph. Mice were administered i.c.v. with Sc.Aβ or Aβ25–35 peptide (9 nmol) and killed 1, 3, 5, 7 days after injection. ANOVA: n=9–15 per group, F(4,60)=4.02, p<0.01 in (b); n=7–12, F(4,42)=2.71, p<0.05 in (c); n=6–8, F(4,37)=3.23, p<0.05 in (d). *p<0.05, **p<0.01, ***p<0.001 vs the Sc.Aβ-treated group; Dunnett’s test.
The time-course analysis of Akt phosphorylation showed that significant decreases are observed at day 1 and 3 after Aβ25–35 injection as compared with Sc.Aβ controls (Figure 1b). The levels then progressively returned to control values. At day 7, a 15% decrease was still observable, but the comparison with Sc.Aβ controls failed to reach significance. The time-course analysis of GSK-3β phosphorylation showed a significant decrease of the P(Ser9)GSK-3β/GSK-3β ratio only at day 7 after peptide injection. However, the phosphorylation on Tyr216 rapidly and highly significantly increased at all times tested after the peptide injection. The protein loading and variation of the total kinase levels were checked using β-tubulin, and neither Akt nor GSK-3β expression was changed after Aβ25–35 injection (F(4,37)=1.24, p>0.05 in Figure 1b and F(4,43)=0.51, p>0.05 in Figure 1c).
Although causal relationships remained hazardous from ex vivo measures, these observations indicated in a coherent manner that the Aβ25–35 injection provokes, within days after i.c.v. injection in mice, an inhibition of the phosphatidyl-inositol 3-kinase (PI3K)/Akt pathway leading to or reinforcing the activation of GSK-3β.
GSK-3β Activation is Involved in Aβ25–35-induced Toxicity and Memory Impairments
In order to determine whether this Akt inactivation and GSK-3β activation could be deleterious, we treated animals with the GSK-3β inhibitor Tibpo, i.c.v. simultaneously with Aβ25–35 peptide. The level of oxidative stress in the hippocampus was analyzed 9 days after injections (Figure 2a), in animals that were previously evaluated at the behavioral level on day 7 using spontaneous alternation in the Y-maze, a spatial working memory procedure (Figure 2b) and on days 8 and 9 using passive avoidance, a long-term contextual procedure (Figure 2c and d). A second batch of animals was tested at days 6–8 after injection in the novel object recognition procedure, a recognition memory highly impacted in AD (Figure 2e and f).
Protective effect of Tibpo against Aβ25–35-induced toxicity and learning impairments in mice. (a) Lipid peroxydation levels in the mouse hippocampus; (b) spontaneous alternation performances; (c) step-through latency; and (d) escape latency in the passive avoidance test; (e) day 1 session and (f) day 2 session in the novel object recognition test. Mice were administered with Tibpo (0.03–1 nmol i.c.v.) or the vehicle solution (V) immediately before the i.c.v. injection of scrambled Aβ25–35 or Aβ25–35 peptide (9 nmol i.c.v.) at day 0. At day 7, they were tested for spontaneous alternation, at days 8 and 9, for passive avoidance response and killed. Their hippocampus was used for lipid peroxydation measure. Another batch of animals was used at days 6–8 for the novel object recognition test in (e, f). Data show the preferential exploration index calculated as the ratio of number of contact with the object in position #2 over the total number of contacts with the two objects, expressed as percentage. The number of mice per group was n=6 in (a), n=10 in (b–d), n=11–12 in (e, f). F(5,35)=10.9, p<0.0001 in (a); F(6,57)=5.61, p<0.001 in (b); H=31.4, p<0.0001 in (c); H=28.1, p<0.0001 in (d). *p<0.05, **p<0.01 vs the (Sc.Aβ+V)-treated group; ##p<0.01 vs the (Aβ25–35+V)-treated group; Dunnett’s test in (a, b); Dunn’s test in (c, d). Op<0.05, OOp<0.01 vs 50% level, one-sample t-test in (f).
Aβ25–35 provoked a +50% increase in lipid peroxydation levels that was prevented by Tibpo, with significant differences observed at the 0.3 and 1 nmol i.c.v. doses (Figure 2a). The Tibpo treatment led to a dose-dependent, bell-shaped prevention of the appearance of Aβ25–35-induced alternation deficits, with significant effects observed for the doses of 0.1 and 0.3 nmol (Figure 2b). In the passive avoidance test, the Aβ25–35-induced deficit in step-through latency and increase in escape latency were corrected by the drug, at the doses of 0.1, 0.3, and 1 nmol in a highly significant manner (Figure 2c and d).
None of the treatment group affected the exploration of the two identical objects during the session 2 of the novel object recognition test, resulting in a 50% contacts for the object in position #2 (Figure 2e). During session 3, Aβ25–35-treated mice failed to preferentially explore the novel object, contrarily to Sc.Aβ-treated mice (Figure 2f). The Tibpo treatment dose-dependently prevented the recognition memory deficit, with highly significant differences at the doses of 0.3 and 1 nmol (Figure 2f). The GSK-3β inhibitor was ineffective at the highest dose tested in Sc.Aβ-treated mice on all responses. These data showed that GSK-3β activation is directly involved in the Aβ25–35-induced toxicity and behavioral deficits in mice.
The GSK-3β Inhibitor Tibpo Blocked GSK-3β Activation and Tau Hyperphosphorylation in Aβ25–35-injected Mice
At the active dose of 0.3 nmol i.c.v., we observed that Tibpo blocked the Aβ25–35-induced increase in GSK-3β phosphorylation on Tyr216 in the mouse hippocampus (Figure 3b), with concomitantly no change in GSK-3β phosphorylation on Ser9 (Figure 3a). We analyzed the levels of hyper- and abnormal phosphorylation of Tau protein induced by Aβ25–35 in the hippocampus by using AT8 antibody, which recognizes, specifically P(Ser202,Thr205)Tau, a physiological epitope of Tau phosphorylation, and AT100 antibody, which recognize, specifically P(Ser212, Thr214) Tau, a pathological phosphorylation epitope. The Aβ25–35 treatment highly significantly increased AT8 immunoreactivity (+236%, Figure 3c) and AT100 labelling (+82%, Figure 3d). The Tibpo treatment significantly blocked both increases in AT8 and AT100 immunoreactivities (Figure 3c and d).
Effect of the GSK-3β inhibitor Tibpo on GSK-3β activity and the hyper- and abnormal phosphorylation of Tau protein 7 days after Aβ25–35 injection in mice. (a) P(Ser9)GSK-3β/GSK-3β ratio, (b) P(Tyr216)GSK-3β/GSK-3β ratio, (c) P(Ser202,Thr205)Tau/Tau ratio, and (d) P(Ser212, Thr214)Tau/Tau ratio. Mice were administered with Tibpo (0.3 nmol i.c.v.) or the vehicle solution (V) immediately before the i.c.v. injection of Sc.Aβ or Aβ25–35 peptide (9 nmol i.c.v.), 7 days before killing. The number of mice per group was n=4 in (a, b) and 10–12 in (c, d). F<1 in (a); F(3,15)=3.55, p<0.05 in (b); F(3,43)=28.1, p<0.0001 in (c); F(3,69)=4.05, p<0.05 in (d). *p<0.05, **p<0.01 vs the (Sc.Aβ+V)-treated group; #p<0.05, ##p<0.01 vs the (Aβ25–35+V)-treated group; Dunnett’s test.
We therefore confirmed that Aβ25–35 injection in mice results in Akt inactivation, GSK-3β activation, Tau phosphorylation, toxicity, and behavioral impairments and that this coherent scheme occurred in a GSK-3β-dependent manner.
ANAVEX2-73, and the Reference Ligands PRE-084 and Xanomeline, Blocked Aβ25–35-induced Recognition Memory Deficits
The second part of the study consisted in the determination of the protective effect of ANAVEX2-73 on Tau phosphorylation and Aβ1–42 seeding, in comparison with two reference muscarinic and σ1 receptor agonists, namely xanomeline and PRE-084, respectively. The different drugs have been previously tested in several behavioral procedures, including spontaneous alternation and passive avoidance (Meunier et al, 2006; Villard et al, 2011), but never using novel object recognition. We used this procedure to determine the most active doses of the three drugs to be selected in biochemical analyses. Analysis of the total locomotor activity and percentage of presence in the centre of the open field during session 1, revealed no treatment effect. Animals treated with Aβ25–35 and ANAVEX2-73 (0.1, 0.3, or 1 mg/kg i.p.), Aβ25–35 and PRE-084 (0.5 or 1 mg/kg i.p.), or Aβ25–35 and xanomeline (0.5 or 1 mg/kg i.p.) walked about 60 m in 10 min and spent about 20% of the time in the central 25 × 25 cm2 square of the open field (data not shown). During session 2, analysis of object exploration showed no preference between the two identical objects in Aβ25–35-injected mice and after the ANAVEX2-73 treatment (Figure 4a). However, during session 3, Aβ25–35-treated mice failed to show a preferential exploration of the novel object, as compared with Sc.Aβ-treated mice (Figure 4b). The ANAVEX2-73 treatment dose-dependently blocked the recognition memory deficit, with a significant effect measured at 1 mg/kg (Figure 4b). Animals treated with PRE-084 failed to show any difference in object exploration during session 2 (Figure 4c), but also showed a significant reversion of the Aβ25–35-induced deficits during session 3, at the dose of 1 mg/kg (Figure 4d). Finally, the xanomeline treatment also showed no difference among groups in session 2 (Figure 4e), but the drug alleviated the Aβ25–35-induced deficits in session 3, with a significant effect at the lowest dose tested (Figure 4f). These behavioral data confirmed that selective or mixed σ1 receptor agonists and M1 cholinergic receptor agonists are able to prevent the Aβ25–35-induced learning impairment when they were injected at the same time as the peptide. These different treatment groups were then used for biochemical analysis of the hyperphosphorylation of Tau and Aβ1–40/42 generation.
Effect of (a, b) ANAVEX2-73, (c, d) PRE-084, and (e, f) xanomeline in the novel object recognition procedure in Aβ25–35-treated mice: (a, c, e) day 1 session, (b, d, f) day 2 session. Animals were treated i.p. with ANAVEX2-73 (0.1, 0.3, 1 mg/kg), PRE-084 (0.5, 1 mg/kg), xanomeline (0.5, 1 mg/kg), or saline solution (V), 20 min before the Aβ25–35 or Sc.Aβ (9 nmol) i.c.v. injection, at day 0. At day 6–8, they were used for the novel object recognition test. Data showed the preferential exploration index calculated as the ratio of number of contact with the object in position #2 over the total number of contacts with the two objects, expressed as percentage. n=13–15 per group, Op<0.05, OOp<0.01 vs 50% level, one-sample t-test.
The Drug Treatments Prevented Alterations in Kinase Activity and Tau Hyperphosphorylation
The impact of the drug treatments was first analyzed on Aβ25–35-induced decrease in Akt phosphorylation on Ser473 at 1 and 7 days after the peptide injection (Figure 5). One day after injections, a significant 32–34% decrease in Akt phosphorylation was measured, which was significantly attenuated by ANAVEX2-73 at 0.1 and 1 mg/kg dose (Figure 5a), PRE-084 at 1 mg/kg (Figure 5b), and xanomeline at 0.5 mg/kg (Figure 5c). Akt phosphorylation was still significantly decreased by 16–18% 7 days after injection. The ANAVEX2-73 treatment resulted only in a non-significant attenuation of the decrease in P(Ser473)Akt/Akt ratio at 0.1 and 0.3 mg/kg (Figure 5d). At day 7, PRE-084 and xanomeline significantly blocked the decrease in P(Ser473)Akt/Akt ratio both at the dose of 1 mg/kg, each (Figure 5e and f, respectively).
Effect of ANAVEX2-73 (a, d), PRE-084 (b, e), and xanomeline (c, f) on Akt phosphorylation in the hippocampus, 1 or 7 days after Aβ25–35 injection in mice: P(S473)Akt/total Akt ratio. Mice were administered with ANAVEX2-73 (0.1–1 mg/kg i.p.), PRE-084 (0.5, 1 mg/kg i.p.), xanomeline (0.5, 1 mg/kg i.p.), or saline (V) 20 min before the Aβ25–35 or Sc.Aβ (9 nmol) i.c.v. injection, 1 day before killing. n=7–8, F(4,25)=4.23, p<0.05 in (a); n=6–9, F(3,28)=3.39, p<0.05 in (b); n=4–9, F(3,25)=4.47, p<0.05 in (c); n=10–13, F(4,55)=3.32, p<0.05 in (d); n=5–13, F(3,35)=3.61, p<0.05 in (e); n=5–9, F(3,27)=6.92, p<0.01 in (f). *p<0.05, **p<0.01 vs the (Sc.Aβ+V)-treated group; #p<0.05, ##p<0.01 vs the (Aβ25–35+V)-treated group; Dunnett’s test.
Seven days after injections, ANAVEX2-73 attenuated the decrease in Ser9 phosphorylation induced by the peptide at 0.3 and 1 mg/kg (Figure 6a), but not significantly as compared with the Aβ25–35/Veh-treated group. The drug blocked the Aβ25–35-induced increase in P(Tyr216)GSK-3β, with a significant effect at the three highest doses tested (Figure 6b). PRE-084 failed to affect the decrease in P(Ser9)GSK-3β significantly (Figure 6c), but significantly blocked the increase in P(Tyr216)GSK-3β at the 1 mg/kg dose (Figure 6d). The xanomeline treatment led to a significant blockade of the decrease in P(Ser9)GSK-3β induced by Aβ25–35 (Figure 6e), at the dose of 1 mg/kg, and to a blockade of P(Tyr216)GSK-3β but with a significant effect measured for the lowest, 0.5 mg/kg, dose (Figure 6f).
Effect of ANAVEX2-73 (a, d), PRE-084 (b, e), and xanomeline (c, f) on GSK-3β phosphorylation in the hippocampus, 7 days after Aβ25–35 injection in mice. (a–c) P(Ser9)GSK-3β/total GSK-3β ratio and (d–f) P(Tyr216)GSK-3β/total GSK-3β ratio. Mice were administered with ANAVEX2-73 (0.1–1 mg/kg i.p.), PRE-084 (0.5, 1 mg/kg i.p.), xanomeline (0.5, 1 mg/kg i.p.), or saline (V) 20 min before the Aβ25–35 or Sc.Aβ (9 nmol) i.c.v. injection, 7 days before killing. n=7–12, F(4,45)=2.81, p<0.05 in (a); n=5–15, F(3,41)=2.91, p<0.05 in (b); n=5–12, F(3,32)=5.09, p<0.01 in (c); n=7–9, F(4,41)=2.62, p<0.05 in (d); n=5–14, F(3,36)=4.28, p<0.05 in (e); n=5–9, F(3,27)=9.51, p<0.001 in (f). *p<0.05, ** p<0.01, ***p<0.001 vs the (Sc.Aβ+V)-treated group; #p<0.05, ##p<0.01 vs the (Aβ25–35+V)-treated group; Dunnett’s test.
Consequently, the drug treatments impacted the Aβ25–35-induced increases in Tau phosphorylation (Figure 7). ANAVEX2-73 dose-dependently and significantly blocked Tau phosphorylation on (Ser202,Thr205) epitopes (Figure 7a) and significantly but partially reversed Tau phosphorylation on (Ser212,Thr214) epitopes (Figure 7b). PRE-084 blocked both Aβ25–35-induced increases in Tau phosphorylation, significantly at the dose of 1 mg/kg (Figure 7c and d). Xanomeline appeared more effective at the lowest dose on P(Ser202,Thr205)Tau and at the highest dose tested on P(Ser212,Thr214)Tau (Figure 7e and f), but with significant effects in each case. It therefore appeared that all the drug treatments, ie, using the non-selective σ1/muscarinic drug ANAVEX2-73, the σ1 selective agonist PRE-084 or the selective muscarinic ligand xanomeline, could efficiently block the pathological Tau hyper-phosphorylation and related kinase pathways induced by Aβ25–35 in mice.
Effect of ANAVEX2-73 (a, b), PRE-084 (c, d), and xanomeline (e, f) on hyper- and abnormal phosphorylation of Tau protein in the hippocampus, 7 days after Aβ25–35 injection in mice. (a, c, e) P(Ser202,Thr205)Tau/total Tau ratio and (b, d, f) P(Ser212, Thr214)Tau/total Tau ratio. Mice were administered with ANAVEX2-73 (0.1–1 mg/kg i.p.), PRE-084 (0.5, 1 mg/kg i.p.), xanomeline (0.5, 1 mg/kg i.p.), or saline 20 min before the Aβ25–35 or Sc.Aβ (9 nmol) i.c.v. injection, 7 days before killing. n=7–14, F(4,45)=4.58, p<0.01 in (a); n=12–17, F(4,75)=3.59, p=0.01 in (b); n=5–7, F(3,22)=10.5, p<0.001 in (c); n=5–11, F(3,35)=4.14, p<0.05 in (d); n=5–7, F(3,24)=3.88, p<0.05 in (e); n=4–14, F(3,36)=3.98, p<0.05 in (f). *p<0.05, **p<0.01, ***p<0.001 vs the (Sc.Aβ+V)-treated group; #p<0.05, ##p<0.01 vs the (Aβ25–35+V)-treated group; Dunnett’s test.
Effect of Drug Treatments on Aβ1–42 Seeding in Aβ25–35-treated Mice
As we previously reported (Meunier et al, 2013), a significant 35–42% increase in endogenous Aβ1–42 content could be measured 7 days after Aβ25–35 injection in the mouse hippocampus, as compared with Sc.Aβ-treated animals (Figure 8a–c). The peptide injection failed, however, to affect endogenous Aβ1–40 content (Figure 8b).
Effect of ANAVEX2-73, PRE-084, and xanomeline on Aβ1–42 and Aβ1–40 contents measured by ELISA assay in the hippocampus, 7 days after Aβ25–35 injection in mice. (a) Effect of ANAVEX2-73 on Aβ25–35-induced increase in Aβ1–42 content; (b) lack of effect of Aβ25–35 on Aβ1–40 content; (c) effect of PRE-084 on Aβ25–35-induced increase in Aβ1–42 content; (d) effect of xanomeline on Aβ25–35-induced increase in Aβ1–42 content. Mice were administered with ANAVEX2-73 (0.1–1 mg/kg i.p.), PRE-084 (0.5, 1 mg/kg i.p.), xanomeline (0.5, 1 mg/kg i.p.), or saline (V) 20 min before the Aβ25–35 or Sc.Aβ (9 nmol) i.c.v. injection, 7 days before killing. n=6–9, F(4,31)=7.43, p<0.05 in (a); n=6, t=0.12, p>0.05 in (b); n=6–7, F(3,24)=4.58, p<0.05 in (c); n=6, F(3,23)=6.65, p<0.01 in (d). *p<0.05, ** p<0.01, ***p<0.001 vs the (Sc.Aβ+V)-treated group; #p<0.05, ###p<0.001 vs the (Aβ25–35+V)-treated group; Dunnett’s test.
The ANAVEX2-73 treatment dose-dependently prevented the Aβ25–35-induced increase in Aβ1–42 content, with a significant effect at the highest dose tested (Figure 8a). Interestingly, the drug did not lower the Aβ1–42 level below baseline. Both PRE-084 and xanomeline also significantly attenuated the Aβ25–35-induced increase in Aβ1–42 content with a significant effect at their lower dose tested (Figure 8c and d). The induction of amyloidogenic pathway was also analyzed using western blot by measuring the C99 fragment produced by β-secretase cleavage of APP. Aβ25–35 induced a significant 40–49% increase in C99 expression (Figure 9a–c). The ANAVEX2-73 treatment dose-dependently prevented the Aβ25–35-induced increase in C99 level, with highly significant effects at 0.3 and 1 mg/kg (Figure 9a). PRE-084 failed to affect C99 expression (Figure 8b), but xanomeline significantly prevented the Aβ25–35-induced increase in C99 expression at the highest dose tested (Figure 9c). These observations concomitantly suggested that ANAVEX2-73 is able to alleviate endogenous Aβ1–42 seeding induced by Aβ25–35 in mice, both by its muscarinic and σ1 properties.
Effect of ANAVEX2-73 (a), PRE-084 (b), and xanomeline (c) on amyloid C99 fragment level in the hippocampus, 7 days after Aβ25–35 injection in mice. Mice were administered with ANAVEX2-73 (0.1–1 mg/kg i.p.), PRE-084 (0.5, 1 mg/kg i.p.), xanomeline (0.5, 1 mg/kg i.p.), or saline (V) 20 min before the Aβ25–35 or Sc.Aβ (9 nmol) i.c.v. injection, 7 days before killing. n=6–8, F(4,33)=6.50, p<0.001 in (a); n=10–12, F(3,20)=3.47, p<0.05 in (b); n=10–12, F(3,21)=3.59, p<0.05 in (c). *p<0.05, ***p<0.001 vs the (Sc.Aβ+V)-treated group; #p<0.05, ##p<0.01 vs the (Aβ25–35+V)-treated group; Dunnett’s test.
DISCUSSION
The main finding in this study is that new therapeutic pathways can be found to alleviate the Tau pathology and amyloid seeding in AD using unconventional targets. We used, here, a mouse model where Aβ25–35 i.c.v. injection in mice results in kinase activation and Tau phosphorylation, on one hand, and increased levels of Aβ1–42 in the mouse hippocampus, on the other hand. Based on this model, we confirmed the central role of GSK-3β in the toxicity as drugs acting directly, as GSK-3β inhibitor, or indirectly, as muscarinic and/or σ1 ligands, can efficiently alleviate these two major alterations observed in Aβ25–35-injected mice, as well as in AD patient brains. More interestingly, the mixed muscarinic and σ1 agonist ANAVE2-73 exhibited powerful effects despite its moderate affinity for these receptors, emphasing its great advantage for therapy.
Aβ25–35 Injection in Mice Results in Hyperphosphorylation of Tau
Dysfunction of GSK-3 is implicated in several human diseases, including AD, Parkinson’s disease, or cancer. The activity of GSK-3 is dependent on phosphorylation at specific sites: phosphorylation on Ser9 (for GSK-3β) or Ser21 (for GSK-3α) inhibits activity, whereas phosphorylation of Tyr216 (for GSK-3β) or Tyr279 (for GSK-3α) increases activity. Although it does not constitute a direct measure, analysis of the phosphorylation levels on these epitopes has been shown to correctly reflect the kinase activity (Dajani et al, 2001; Kockeritz et al, 2006; Kremer et al, 2011). GSK-3β is the main isoform involved in AD pathology. It must be outlined that inhibition of GSK-3β has more influence on activity than activation, as the enzyme is constitutively active and activation sites are subjected to autophosphorylation (Cole et al, 2004). One of the most characterized regulation pathways for GSK-3β is through protein kinase B (Akt) activation. Several receptors for neurotransmitters and neurotrophic factors, coupled to PI3K that phosphorylates Akt, in turn inhibit GSK-3β through phosphorylation of Ser9 residue (Liu et al, 2003). Other kinases such as PKC can also inhibit GSK-3β activity by phosphorylating Ser9 (Liu et al, 2003) and this inhibition by PKC is additive to the inhibition by Akt.
Amyloid peptides, and particularly Aβ25–35, have been reported to regulate Akt and GSK-3β activities, either in vitro (Yin et al, 2005) or in vivo. For instance, 12 days after Aβ25–35, the levels of P(Ser473)-Akt/Akt ratio were decreased in ICR mice, an effect blocked by the σ1 receptor agonist dehydroepiandrosterone (DHEA; Li et al, 2010). This effect was accompanied by a decrease in mTOR phosphorylation, clearly involving a diminution of the PI3K/Akt/mTOR pathway in Aβ25–35-induced toxicity. In turn, Aβ provokes the hyperphosphorylation of Tau. Alternative mechanisms may, however, also be involved, including oxidative stress (Mattson et al, 1997), perturbed cellular Ca2+ homeostasis (Mattson, 2004), activation of other kinases, or inhibition of phosphatases (Stoothoff and Johnson, 2005). In the present study, we confirmed that the i.c.v. injection of Aβ25–35 resulted in a rapid, highly significant reduction of the P(Ser473)-Akt/Akt ratio, within 1 to 2 days after injection. Interestingly, we also observed a significant, but very transient, decrease in total Akt level, one day after the peptide injection (data not detailled). Other authors have reported, using combined microarray and RT-PCR analyses of gene expression profiles that Akt is downregulated in the cortex of Balb/c mice 14 days after i.c.v. Aβ25–35 injection, at a dose that impeded water-maze learning (Kong et al, 2005). Our results, however, suggested that the downregulation of Akt activity is an earlier event, appearing within days after the peptide injection and participating in the subsequent disorder of signalling pathways.
Indeed, GSK-3β activity appeared altered by Aβ25–35. Klementiev et al (2007) first reported that in rat cingulate cortex, not only total GSK-3β and P(Tyr216)-GSK-3β, but also P(Ser9)-GSK-3β were increased after Aβ25–35 injection. We could observe an increase in P(Tyr216)-GSK-3β/GSK-3β ratio, but not in P(Ser9)-GSK-3β/GSK-3β ratio. By contrast, the latter diminished gradually with time after Aβ25–35 injection. These effects both signed an increase in GSK-3β activity that appeared long-lasting over the 7 days of measure. The time course was therefore different to what could be expected from the previous observation on Akt activity, suggesting that Akt is not the only kinase involved in the amyloid peptide effect on GSK-3β. Aβ could therefore accelerate Tau phosphorylation by several mechanisms, notably GSK-3β activation (Takashima et al, 1993, 1996, 1998). It has indeed been shown that Aβ25–35 treatment activated Tau, GSK-3β, but not GSK-3α or mitogen-activated protein kinase (MAP kinase), in primary culture of rat hippocampal neurons. In addition, treatment of the cultures with a GSK-3β-targeting antisense oligonucleotide inhibited the enhancement of Tau phosphorylation induced by Aβ25–35 exposure (Takashima et al, 1998). Such observation clearly confirmed the specificity of the role of GSK-3β in amyloid toxicity and in linking amyloid toxicity and Tau hyperphosphorylation.
A GSK-3β Inhibitor Alleviates Aβ25–35-induced Toxicity and Memory Deficits
The confirmation of the importance of GSK-3β activation in the amyloid toxicity must come from the demonstration of a therapeutic effect for agents (oligonucleotides or small molecules) that inhibit GSK-3β activity in vivo. We used Tibpo, an oxadiazole derivative inhibiting GSK-3β activity with an IC50 of 390 nM (Naerum et al, 2002). It was previously reported to increase the viability of cells transfected with G93A- or A4V-mutant types of human Cu/Zn-superoxyde dismutase gene, both lines being models of familial amyotrophic lateral sclerosis. This pro-survival effect relied on the activation of heat shock transcription factor-1 and reduction in cytochrome c release, caspase-3 activation, and poly(ADP-ribose) polymerase cleavage (Koh et al, 2005). In our model, the compound blocked the Aβ25–35-induced phosphorylation of GSK-3β on Tyr216, and the induction of Tau phosphorylation, examined on Ser202,Thr205 or Ser212,Thr214 epitopes, using AT8 or AT100 anti-phospho-Tau antibody, respectively. It dose-dependently prevented the Aβ25–35-induced oxidative stress in the hippocampus and memory alterations, in terms of spontaneous alternation, passive avoidance or object recognition, so affecting spatial and non-spatial, short- and long-term memories. We clearly measured the importance of GSK-3β activation in Aβ toxicity and the pharmacological potential of such GSK-3β inhibitors. Indeed, an orally administrable-related oxidiazole, 2-methyl-5-(3-{4-[(S)-methylsulfinyl]phenyl}-1-benzofuran-5-yl)-1,3,4-oxadiazole (MMBO), was recently shown to decrease hippocampal Tau phosphorylation at GSK-3 sites, but without affecting Aβ pathology, in the 3xTg transgenic AD mouse model. In behavioral assessments, MMBO significantly improved memory deficits in the Y-maze and novel object recognition tests (Onishi et al, 2011). Therefore, these molecules appeared effective in preclinical tests. Their use in clinical trials may, however, be impeded by adverse effects due to the numerous cellular roles of GSK-3β.
The Mixed Muscarinic/σ1 Ligand ANAVEX2-73 Prevent Tau Hyperphosphorylation in Aβ25–35-injected Mice
The main purpose of the present study was to analyze ANAVEX2-73 effects on Tau pathology and Aβ accumulation, by comparison with the reference and selective σ1 receptor agonist PRE-084 (Su et al, 1991) and the muscarinic ligand xanomeline, devoid of σ1 activity. Xanomeline has high affinity for M1 receptors (IC50=7 nM) as measured by the inhibition of [3H]-pirenzepine binding in hippocampal and cortical membranes (Shannon et al, 1994). It also has high affinity for inhibiting the binding of [3H]-oxotremorine (IC50=3 nM), but is 10- to 20-fold less potent in inhibiting [3H]-quinuclidinyl benzilate binding (IC50=70 nM) at M2 receptors in brain stem and forebrain membranes (Shannon et al, 1994), a pharmacological profile comparable to ANAVEX2-73 but at higher affinities. The drug was already proven to be effective in patients with probable AD (Bodick et al, 1997). We first confirmed that the three drugs attenuated the Aβ25–35-induced behavioral impairments at low mg/kg doses, by using the novel object recognition procedure. Recognition memory is indeed rapidly and drastically degraded in AD patients. The efficacy of these drugs in the procedure was not previously reported. It confirmed the active dose range observed using the spontaneous alternation and passive avoidance procedures for PRE-084 (Meunier et al, 2006) or ANAVEX2-73 (Villard et al, 2011). It also showed that xanomeline is active in the model in the dose range. We then reported that the decreases in P(Ser473)-Akt/Akt ratios, measured significantly at day 1 and 7 after Aβ25–35, could be blocked by the three drugs at their behaviorally active doses. The resulting decrease in GSK-3β phosphorylation on Ser9 was significantly blocked only by xanomeline but attenuated by ANAVEX2-73 and PRE-084. The three drugs, however, significantly blocked the Aβ25–35-induced increase in GSK-3β phosphorylation on Tyr216. These effects were consequently associated with blockade of the Aβ25–35-induced Tau hyperphosphorylation on both Ser202,Thr205 and Ser212,Thr214 epitopes.
Muscarinic ligands, and particularly M1 receptor agonists, have been shown attenuate Tau pathology in several models and particularly in 3xTg-AD transgenic mice (Caccamo et al, 2006). The M1 selective ligand (S)-2-ethyl-8-methyl-1-thia-4,8-diazaspiro[4.5]decan-3-one (AF267B) reduced the Tau pathology in the hippocampus and cortex of the mice, the HT7 and AT8 immunoreactivities in the same brain structures, and GSK-3β activity (Caccamo et al, 2006). This last effect was directly attributable to an increase in PKC activity induced by AF267B. Indeed, Aβ25–35 not only decreases Akt activity but also PKC activity in the hippocampus and cortex (Olariu et al, 2001). The efficacy of xanomeline in our model is therefore not surprising. It was clearly proposed that muscarinic ligands, through their ability to directly activate the PLC/PKC pathway, could very efficiently decrease the hyper-activation of GSK-3β in AD (Fisher, 2008, 2012).
The efficacy of a selective σ1 receptor ligand, like PRE-084, could also involve a facilitation of the PLC/PKC pathway. It was indeed shown that antidepressants (imipramine) enhance the brain-derived neurotrophic factor signalling on the PLC-γ/IP3/Ca2+ pathway via activation of the σ1 receptor in primary rat neuron cultures (Yagasaki et al, 2006). Moreover, Nakano et al (2010) directly demonstrated that the antidepressant (fluvoxamine) effect relied on a rapid increase in phosphorylation of Akt, as mimicked by brain-derived neurotrophic factor itself or by the σ1 receptor agonist DHEA sulfate. Our results, and the recent demonstration that both DHEA and pregnenolone sulfate prevented Aβ25–35 toxicity through a modulation of the PI3K/Akt/mTOR signalling (Li et al, 2010; Yang et al, 2012), confirmed the in vivo efficacy of σ1 ligand to modulate GSK-3β activity. A direct interaction has not been shown yet, but it may involve either modulation of PKC activity or regulation of Ca2+ mobilization from the ER. As calcineurin, a major calcium-dependent protein phosphatase, has been shown to be able to dephosphorylate GSK-3β at Ser9 (Kim et al, 2009), local changes in Ca2+, as the ones gated by the σ1 protein (Hayashi et al, 2000), could modulate the kinase activity.
The Mixed Muscarinic/σ1 Ligand ANAVEX2-73 Prevent Aβ1–42 Seeding in Aβ25–35-injected Mice
We finally examined whether the drug treatments could also prevent the endogenous accumulation in Aβ. It has been repeatedly shown that the i.c.v. injection of Aβ25–35 in rats and mice increases β-secretase activity and Aβ levels in the hippocampus and cortex of the animals (Klementiev et al, 2007; Chavant et al, 2010; Zussy et al, 2011). All treatments resulted in a significant blockade of Aβ25–35-induced increase in Aβ1–42 levels measured by ELISA. When we analyzed the increase in C99 levels, PRE-084 appeared, however, less effective. Globally, the data suggested that the muscarinic activity of the compound is mainly involved in their ability to reduce the amyloid load in Aβ25–35-treated animals. The mechanism involved in this effect may also rely on the PLC/PKC pathway activated by M1 muscarinic receptors, which has been shown to increase the activity of α-secretase, therefore preventing the formation of Aβ (Nitsch et al, 1992). The α-secretase involved is ADAM17, activated by PKCα/ɛ isoforms (Cisse et al, 2011; Fisher, 2012). Moreover, the AF267B treatment in 3xTg-AD transgenic mice, as detailled earlier, induced not only increases in PKC or MAP kinase, but also in ADAM17, accompanied by decreases in Aβ, C99 GSK-3β, and BACE-1 levels (Caccamo et al, 2006). Alternatively, whether σ1 protein activation could modulate secretase activities has not been directly addressed. But it is likely that σ1 ligand could impact Aβ generation by different pathways, including the modulation of PI3K/Akt/PLC signalling as previously outlined. Moreover, secretase activity could be directly modulated by σ1 protein activation. First, isoflurane has been shown to activate BACE-1 via activation of the inositol 1,4,5-trisphosphate receptor, the main target of the σ1 protein, and the resulting Ca2+ deregulation may be a contributing factor in the mechanism of isoflurane-induced neurodegeneration (Zhao et al, 2010). A similar mechanism could be evoked in AD. Second, oxidative stress, known to directly activate the σ1 protein (Meunier and Hayashi, 2010), is associated with Aβ accumulation in the brains of AD patients. Significant amounts of BACE-1 and γ-secretase components localize in the cholesterol-rich region of membranes known as lipid rafts, where Aβ production occurs preferentially and where σ1 protein accumulate after overactivation (Hayashi and Su, 2001, 2003). Oda et al (2010) observed that an oxidative stress enhanced presenilin-1 protein levels, a component of the γ-secretase complex, in lipid rafts via upregulation of its transcription. This effect may constitute the mechanism underlying the oxidative stress-associated promotion of Aβ production (Oda et al, 2010), a mechanism likely to constitute the direct target of σ1 ligands.
Finally, our present data confirmed the pharmacological potentiality of mixed compounds, like ANAVEX2-73. The compound, although presenting a micromolar order of affinity for its pharmacological targets, showed a similar active dose as compared with the two selective compounds, both presenting nanomolar affinities for the muscarinic or σ1 receptor, allowing to limit the adverse effects usually observed with pure muscarinic receptor ligands. The present data clearly suggested that both receptors target GSK-3β activity and that inhibiting this kinase efficiently decreased Tau hyperphosphorylation and Aβ accumulation in the AD model. These treatments are currently tested in AD transgenic mice, where the ability of the drugs to protect brain neurons degenerating in AD, together with an expected limitation of the Tau pathology and Aβ seeding, could ultimately lead to a consequent disease-modifying activity.
References
Akiyama H, Shin RW, Uchida C, Kitamoto T, Uchida T (2005). Pin1 promotes production of Alzheimer’s amyloid β from β-cleaved amyloid precursor protein. Biochem Biophys Res Commun 336: 521–529.
Beurel E, Jope RS (2006). The paradoxical pro- and anti-apoptotic actions of GSK-3 in the intrinsic and extrinsic apoptosis signalling pathways. Prog Neurobiol 79: 173–189.
Bhat RV, Budd Haeberlein SL, Avila J (2004). Glycogen synthase kinase 3: a drug target for CNS therapies. J Neurochem 89: 1313–1317.
Bhat RV, Shanley J, Correll MP, Fieles WE, Keith RA, Scott CW et al (2000). Regulation and localization of tyrosine216 phosphorylation of glycogen synthase kinase-3β in cellular and animal models of neuronal degeneration. Proc Natl Acad Sci USA 97: 11074–11079.
Bodick NC, Offen WW, Levey AI, Cutler NR, Gauthier SG, Satlin A et al (1997). Effects of xanomeline, a selective muscarinic receptor agonist, on cognitive function and behavioral symptoms in Alzheimer disease. Arch Neurol 54: 465–473.
Caccamo A, Oddo. S, Billings LM, Martinez-Coria H, Fisher A, LaFerla FM (2006). M1 receptors play a central role in modulating AD-like pathology in transgenic mice. Neuron 49: 671–682.
Cai Z, Zhao Y, Zhao B (2012). Roles of Glycogen synthase kinase 3 in Alzheimer’s disease. Curr Alzheimer Res 9: 864–879.
Chavant F, Deguil J, Pain S, Ingrand I, Milin S, Fauconneau B et al (2010). Imipramine, in part through tumor necrosis factor α inhibition, prevents cognitive decline and β-amyloid accumulation in a mouse model of Alzheimer’s disease. J Pharmacol Exp Ther 332: 505–514.
Cisse M, Braun U, Leitges M, Fisher A, Pages G, Checler F et al (2011). ERK1-independent α-secretase cut of β-amyloid precursor protein via M1 muscarinic receptors and PKCα/ɛ. Mol Cell Neurosci. 2011 47: 223–232.
Cole A, Frame S, Cohen P (2004). Further evidence that the tyrosine phosphorylation of glycogen synthase kinase-3 (GSK3) in mammalian cells is an autophosphorylation event. Biochemical J 377: 249–255.
Dajani R, Fraser E, Roe SM, Young N, Good V, Dale TC et al (2001). Crystal structure of glycogen synthase kinase 3β: structural basis for phosphate-primed substrate specificity and autoinhibition. Cell 105: 721–732.
DaRocha-Souto B, Coma M, Pérez-Nievas BG, Scotton TC, Siao M, Sánchez-Ferrer P et al (2012). Activation of glycogen synthase kinase-3β mediates β-amyloid induced neuritic damage in Alzheimer’s disease. Neurobiol Dis 45: 425–437.
Delobette S, Privat A, Maurice T (1997). In vitro aggregation facilities β-amyloid peptide-(25–35)-induced amnesia in the rat. Eur J Pharmacol 319: 1–4.
Deng J, Shen C, Wang YJ, Zhang M, Li J, Xu ZQ et al (2010). Nicotine exacerbates tau phosphorylation and cognitive impairment induced by amyloid-β25–35 in rats. Eur J Pharmaco 637: 83–88.
Dudas B, Cornelli U, Lee JM, Hejna MJ, Walzer M, Lorens SA et al (2002). Oral and subcutaneous administration of the glycosaminoglycan C3 attenuates Aβ25–35-induced abnormal tau protein immunoreactivity in rat brain. Neurobiol Aging 23: 97–104.
Espallergues J, Lapalud P, Christopoulos A, Avlani VA, Sexton PM, Vamvakides A et al (2007). Involvement of the sigma1 (σ1) receptor in the anti-amnesic, but not antidepressant-like, effects of the aminotetrahydrofuran derivative ANAVEX1-41. Br J Pharmacol 152: 267–279.
Fisher A (2012). Cholinergic modulation of amyloid precursor protein processing with emphasis on M1 muscarinic receptor: perspectives and challenges in treatment of Alzheimer’s disease. J Neurochem 120: 22–33.
Fisher A (2008). Cholinergic treatments with emphasis on m1 muscarinic agonists as potential disease-modifying agents for Alzheimer’s disease. Neurotherapeutics 5: 433–442.
Hayashi T, Maurice T, Su TP (2000). Ca2+ signalling via sigma1-receptors: novel regulatory mechanism affecting intracellular Ca2+ concentration. J Pharmacol Exp Ther 293: 788–798.
Hayashi T, Su TP (2001). Regulating ankyrin dynamics: roles of sigma-1 receptors. Proc Natl Acad Sci USA 98: 491–496.
Hayashi T, Su TP (2007). Sigma-1 receptor chaperones at the ER-mitochondrion interface regulate Ca2+ signalling and cell survival. Cell 131: 596–610.
Hayashi T, Su TP (2003). Sigma-1 receptors (σ1 binding sites) form raft-like microdomains and target lipid droplets on the endoplasmic reticulum: roles in endoplasmic reticulum lipid compartmentalization and export. J Pharmacol Exp Ther 306: 718–725.
Hernandez F, Borrell J, Guaza C, Avila J, Lucas JJ (2002). Spatial learning deficit in transgenic mice that conditionally over-express GSK-3β in the brain but do not form tau filaments. J Neurochem 83: 1529–1533.
Hetman M, Cavanaugh JE, Kimelman D, Zhengui X (2000). Role of glycogen synthase kinase-3β in neuronal apoptosis induced by trophic withdrawal. J Neurosci 20: 2567–2574.
Hooper C, Killick R, Lovestone S (2008). The GSK-3 hypothesis of Alzheimer’s disease. J Neurochem 104: 1433–1439.
Hu S, Begum AN, Jones MR, Oh MS, Beech WK, Beech BH et al (2009). GSK-3 inhibitors show benefits in an Alzheimer's disease (AD) model of neurodegeneration but adverse effects in control animals. Neurobiol Dis 33: 193–206.
Kim DH, Park SJ, Kim JM, Jeon SJ, Kim DH, Cho YW et al (2011). Cognitive dysfunctions induced by a cholinergic blockade and Aβ25–35 peptide are attenuated by salvianolic acid B. Neuropharmacology 61: 1432–1440.
Kim HC, Yamada K, Nitta A, Olariu A, Tran MH, Mizuno M et al (2003). Immunocytochemical evidence that amyloid β1–42 impairs endogenous antioxidant systems in vivo. Neuroscience 119: 399–419.
Kim Y, Lee YI, Seo M, Kim SY, Lee JE, Youn HD et al (2009). Calcineurin dephosphorylates glycogen synthase kinase-3β at serine-9 in neuroblast-derived cells. J Neurochem 111: 344–354.
Klementiev B, Novikova T, Novitskaya V, Walmod PS, Dmytriyeva O, Pakkenberg B et al (2007). A neural cell adhesion molecule-derived peptide reduces neuropathological signs and cognitive impairment induced by Aβ25–35 . Neuroscience 145: 209–224.
Kockeritz L, Doble B, Patel S, Woodgett JR (2006). Glycogen synthase kinase-3—an overview of an over-achieving protein kinase. Curr Drug Targets 7: 1377–1388.
Koh SH, Lee YB, Kim KS, Kim HJ, Kim M, Lee YJ et al (2005). Role of GSK-3β activity in motor neuronal cell death induced by G93A or A4V mutant hSOD1 gene. Eur J Neurosci 22: 301–309.
Kong LN, Zuo PP, Mu L, Liu YY, Yang N (2005). Gene expression profile of amyloid β protein-injected mouse model for Alzheimer disease. Acta Pharmacol Sin 26: 666–672.
Kosik KS (1992). Cellular aspects of Alzheimer neurofibrillary pathology. Prog Clin Biol Res 379: 183–193.
Kremer A, Louis JV, Jaworski T, Van Leuven F (2011). GSK3 and Alzheimer’s Disease: Facts and Fiction…. Front Mol Neurosci 4: 17.
Li L, Xu B, Zhu Y, Chen L, Sokabe M, Chen L (2010). DHEA prevents Aβ25–35-impaired survival of newborn neurons in the dentate gyrus through a modulation of PI3K-Akt-mTOR signalling. Neuropharmacology 59: 323–333.
Liu SJ, Zhang AH, Li HL, Wang Q, Deng HM, Netzer WJ et al (2003). Overactivation of glycogen synthase kinase-3 by inhibition of phosphoinositol-3 kinase and protein kinase C leads to hyperphosphorylation of tau and impairment of spatial memory. J Neurochem 87: 1333–1344.
Lu P, Mamiya T, Lu L, Mouri A, Ikejima T, Kim HC et al (2012). Xanthoceraside attenuates amyloid β peptide25–35-induced learning and memory impairments in mice. Psychopharmacology 219: 181–190.
Lucas JJ, Hernandez F, Gomez-Ramos P, Moran MA, Hen R, Avila J (2001). Decreased nuclear beta-catenin, tau hyperphosphorylation and neurodegeneration in GSK-3β conditional transgenic mice. EMBO J 20: 27–39.
Ma T, Hoeffer CA, Capetillo-Zarate E, Yu F, Wong H, Lin MT et al (2010). Dysregulation of the mTOR pathway mediates impairment of synaptic plasticity in a mouse model of Alzheimer’s disease. PLoS One 5: e12845.
Ma T, Tzavaras N, Tsokas P, Landau EM, Blitzer RD (2011). Synaptic stimulation of mTOR is mediated by Wnt signalling and regulation of glycogen synthetase kinase-3. J Neurosci 31: 17537–17546.
Mattson MP, Robinson N, Guo Q (1997). Estrogens stabilize mitochondrial function and protect neural cells against the pro-apoptotic action of mutant presenilin-1. Neuroreport 8: 3817–3821.
Mattson MP (2004). Pathways towards and away from Alzheimer’s disease. Nature 430: 631–639.
Maurice T, Lockhart BP, Privat A (1996). Amnesia induced in mice by centrally administered β-amyloid peptides involves cholinergic dysfunction. Brain Res 706: 181–193.
Maurice T, Su TP, Privat A (1998). Sigma1 (σ1) receptor agonists and neurosteroids attenuate β25–35-amyloid peptide-induced amnesia in mice through a common mechanism. Neuroscience 83: 413–428.
Meunier J, Hayashi T (2010). Sigma-1 receptors regulate Bcl-2 expression by reactive oxygen species-dependent transcriptional regulation of nuclear factor kappaB. J Pharmacol Exp Ther 332: 388–397.
Meunier J, Ieni J, Maurice T (2006). The anti-amnesic and neuroprotective effects of donepezil against amyloid β25–35 peptide-induced toxicity in mice involve an interaction with the σ1 receptor. Br J Pharmacol 149: 998–1012.
Meunier J, Villard V, Givalois L, Maurice T (2013). The γ-secretase inhibitor 2-[(1R)-1-[(4-chlorophenyl)sulfonyl](2,5-difluorophenyl) amino]ethyl-5-fluorobenzenebutanoic acid (BMS-299897) alleviates Aβ1-42 seeding and short-term memory deficits in the Aβ25-35 mouse model of Alzheimer's disease. Eur J Pharmacol 698: 193–199.
Monnet FP, Morin-Surun MP, Leger J, Combettes L (2003). Protein kinase C-dependent potentiation of intracellular calcium influx by sigma1 receptor agonists in rat hippocampal neurons. J Pharmacol Exp Ther 307: 705–712.
Morin-Surun MP, Collin T, Denavit-Saubié M, Baulieu EE, Monnet FP (1999). Intracellular sigma1 receptor modulates phospholipase C and protein kinase C activities in the brainstem. Proc Natl Acad Sci USA 96: 8196–8199.
Naerum L, Nørskov-Lauritsen L, Olesen PH (2002). Scaffold hopping and optimization towards libraries of glycogen synthase kinase-3 inhibitors. Bioorg Med Chem Lett 12: 1525–1528.
Nakano M, Osada K, Misonoo A, Fujiwara K, Takahashi M, Ogawa Y et al (2010). Fluvoxamine and sigma-1 receptor agonists dehydroepiandrosterone (DHEA)-sulfate induces the Ser473-phosphorylation of Akt-1 in PC12 cells. Life Sci 86: 309–314.
Nitsch RM, Slack BE, Wurtman RJ, Growdon JH (1992). Release of Alzheimer amyloid precursor derivatives stimulated by activation of muscarinic acetylcholine receptors. Science 58: 304–307.
Oda A, Tamaoka A, Araki W (2010). Oxidative stress up-regulates presenilin 1 in lipid rafts in neuronal cells. J Neurosci Res 88: 1137–1145.
Onishi T, Iwashita H, Uno Y, Kunitomo J, Saitoh M, Kimura E et al (2011). A novel glycogen synthase kinase-3 inhibitor decreases tau phosphorylation and ameliorates cognitive deficits in a transgenic model of Alzheimer’s disease. J Neurochem 119: 1330–1340.
Olariu A, Tran MH, Yamada K, Mizuno M, Hefco V, Nabeshima T (2001). Memory deficits and increased emotionality induced by beta-amyloid25–35 are correlated with the reduced acetylcholine release and altered phorbol dibutyrate binding in the hippocampus. J Neural Transm 108: 1065–1079.
Peineau S, Taghibiglou C, Bradley C, Wong TP, Liu L, Lu J et al (2007). LTP inhibits LTD in the hippocampus via regulation of GSK-3β. Neuron 53: 703–717.
Ruan CJ, Zhang L, Chen DH, Li Z, Du GH, Sun L (2010). Effects of trans-2,4-dimethoxystibene against the neurotoxicity induced by Aβ25–35 both in vitro and in vivo. Neurosci Res 67: 209–214.
Selkoe DJ (2004). Cell biology of protein misfolding: the examples of Alzheimer’s and Parkinson’s diseases. Nat Cell Biol 6: 1054–1061.
Shannon HE, Bymaster FP, Calligaro DO, Greenwood B, Mitch CH, Sawyer BD et al (1994). Xanomeline: a novel muscarinic receptor agonist with functional selectivity for M1 receptors. J Pharmacol Exp Ther 269: 271–281.
Stepanichev MY, Moiseeva YV, Lazareva NA, Onufriev MV, Gulyaeva NV (2003). Single intracerebroventricular administration of amyloid-β25–35 peptide induces impairment in short-term rather than long-term memory in rats. Brain Res Bull 61: 197–205.
Stepanichev MY, Zdobnova IM, Zarubenko II, Lazareva NA, Gulyaeva NV (2006). Studies of the effects of central administration of β-amyloid peptide (25–35): pathomorphological changes in the Hippocampus and impairment of spatial memory. Neurosci Behav Physiol 36: 101–106.
Stepanichev MY, Zdobnova IM, Zarubenko II, Moiseeva YV, Lazareva NA, Onufriev MV et al (2004). Amyloid-β25–35-induced memory impairments correlate with cell loss in rat hippocampus. Physiol Behav 80: 647–655.
Stoothoff WH, Johnson GV (2005). Tau phosphorylation: physiological and pathological consequences. Biochim Biophys Acta 1739: 280–297.
Su TP, Wu XZ, Cone EJ, Shukla K, Gund TM, Dodge AL et al (1991). Sigma compounds derived from phencyclidine: identification of PRE-084, a new, selective sigma ligand. J Pharmacol Exp Ther 259: 543–550.
Takashima A, Noguchi K, Sato K, Hoshino T, Imahori K (1993). Tau protein kinase I is essential for amyloid β-protein-induced neurotoxicity. Proc Natl Acad Sci USA 90: 7789–7793.
Takashima A, Noguchi K, Michel G, Mercken M, Hoshi M, Ishiguro K et al (1996). Exposure of rat hippocampal neurons to amyloid β peptide (25–35) induces the inactivation of phosphatidyl inositol-3 kinase and the activation of tau protein kinase I/glycogen synthase kinase-3β. Neurosci Lett 203: 33–36.
Takashima A, Honda T, Yasutake K, Yasutake K, Michel G, Murayama O et al (1998). Activation of tau protein kinase I/glycogen synthase kinase-3β by amyloid β peptide (25–35) enhances phosphorylation of tau in hippocampal neurons. Neurosci Res 31: 317–323.
Vamvakides A (2002a). Anticonvulsant and forced swim anti-immobility effects of tetrahydro-N,N-dimethyl-2,2-diphenyl-3-furanemethanamine (AE37): common action mechanism? Ann Pharm Fr 60: 88–92.
Vamvakides A (2002b). Mechanism of action of the tetrahydro-N,N-dimethyl-5,5-diphenyl-3-furanemethanamine, a putative nootropic, anti-epileptic and antidepressant compound. Ann Pharm Fr 60: 415–422.
Villard V, Espallergues J, Keller E, Alkam T, Nitta A, Yamada K et al (2009). Antiamnesic and neuroprotective effects of the aminotetrahydrofuran derivative ANAVEX1-41 against amyloid β25–35-induced toxicity in mice. Neuropsychopharmacology 34: 1552–1566.
Villard V, Espallergues J, Keller E, Vamvakides A, Maurice T (2011). Anti-amnesic and neuroprotective potentials of the mixed muscarinic receptor/sigma1 (σ1) ligand ANAVEX2-73, a novel aminotetrahydrofuran derivative. J Psychopharmacol 25: 1101–1117.
Wang C, Yang XM, Zhuo YY, Zhou H, Lin HB, Cheng YF et al (2012). The phosphodiesterase-4 inhibitor rolipram reverses Aβ-induced cognitive impairment and neuroinflammatory and apoptotic responses in rats. Int J Neuropsychopharmacol 15: 749–766.
Yagasaki Y, Numakawa T, Kumamaru E, Hayashi T, Su TP, Kunugi H (2006). Chronic antidepressants potentiate via sigma-1 receptors the brain-derived neurotrophic factor-induced signalling for glutamate release. J Biol Chem 281: 12941–12949.
Yang R, Chen L, Wang H, Xu B, Tomimoto H, Chen L (2012). Anti-amnesic effect of neurosteroid PREGS in Aβ25–35-injected mice through σ1 receptor- and α7nAChR-mediated neuroprotection. Neuropharmacology 63: 1042–1050.
Yin KJ, Lee JM, Chen H, Xu J, Hsu CY (2005). Aβ25–35 alters Akt activity, resulting in Bad translocation and mitochondrial dysfunction in cerebrovascular endothelial cells. J Cerebral Blood Flow Metab 25: 1445–1455.
Zhao Y, Liang G, Chen Q, Joseph DJ, Meng Q, Eckenhoff RG et al (2010). Anesthetic-induced neurodegeneration mediated via inositol 1,4,5-trisphosphate receptors. J Pharmacol Exp Ther 333: 14–22.
Zussy C, Brureau A, Delair B, Marchal S, Keller E, Ixart G et al (2011). Time-course and regional analyses of the physiopathological changes induced after cerebral injection of an amyloid β fragment in rats. Am J Pathol 179: 315–334.
Acknowledgements
This work was supported by collaboration contracts between Anavex Life Sciences (Pallini, Greece) and Amylgen (Clapiers, France) and between Amylgen and the University of Montpellier 2 (Montpellier, France). V.L. is recipient of a CIFRE PhD funding (ANRT, Paris, France).
Author contributions
VL designed experiments, carried out research, analyzed data, and implemented the manuscript. JM, SM, GN, and LG performed research and corrected the manuscript. SHK provided drug and participated in the design of the study. AV and VV participated in the study design and coordination, provided financial sources, and corrected the manuscript. TM designed experiments, carried out behavioral studies, analyzed data, and wrote the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
JM, SM, and VV are employees of Amylgen. AV is an employee of Anavex Life Sciences. LG is member of the scientific advisory board of Amylgen. TM is a member of the scientific advisory boards of Anavex Life Sciences and Amylgen. Other authors declare no conflict of interest. Amylgen and Anavex (funding sources) were not involved in designing the experiments or analyzing the data.
Rights and permissions
About this article
Cite this article
Lahmy, V., Meunier, J., Malmström, S. et al. Blockade of Tau Hyperphosphorylation and Aβ1–42 Generation by the Aminotetrahydrofuran Derivative ANAVEX2-73, a Mixed Muscarinic and σ1 Receptor Agonist, in a Nontransgenic Mouse Model of Alzheimer’s Disease. Neuropsychopharmacol 38, 1706–1723 (2013). https://doi.org/10.1038/npp.2013.70
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2013.70
Keywords
This article is cited by
-
Amyloid β-based therapy for Alzheimer’s disease: challenges, successes and future
Signal Transduction and Targeted Therapy (2023)
-
Targeting Sigma Receptors for the Treatment of Neurodegenerative and Neurodevelopmental Disorders
CNS Drugs (2023)
-
Metabolic disorder in Alzheimer’s disease
Metabolic Brain Disease (2021)
-
Multi-Target Drug Candidates for Multifactorial Alzheimer’s Disease: AChE and NMDAR as Molecular Targets
Molecular Neurobiology (2021)
-
Effects of the sigma-1 receptor agonist blarcamesine in a murine model of fragile X syndrome: neurobehavioral phenotypes and receptor occupancy
Scientific Reports (2021)