Abstract
Purpose. This study was performed to examine the distribution in the brain interstitial fluid (ISF) and the blood-brain barrier (BBB) transport of baclofen in rats by a microdialysis technique.
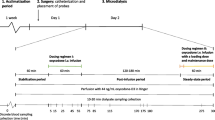
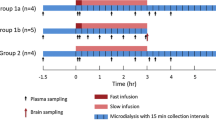
Methods. Following an i.v. bolus administration and/or the constant i.v. infusion of baclofen to the microdialysis cannula-bearing anesthetized rats, the concentrations of baclofen in the hippocampal ISF, whole brain tissue, cerebrospinal fluid (CSF), and plasma were determined by high-performance liquid chromatography (HPLC). Data were kinetically analyzed to estimate the transport parameters, i.e., the influx clearance (CLin) from plasma to brain and the efflux rate constant (keff) from brain to plasma, and the steady-state volume of distribution in the brain (Vd).
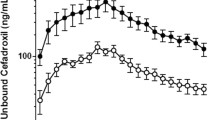
Results. The concentrations of baclofen in ISF, whole brain tissue, and CSF at the pseudo-steady state were almost 30-fold lower than the plasma unbound concentration, suggesting the restricted distribution of baclofen in the brain. The estimated values of CLin and keff were 0.00157 ± 0.00076 ml/min/g of brain and 0.0872 ± 0.0252 min−1, respectively. The efflux clearance (CLout) calculated by multiplying keff by Vd (0.816 ± 0.559 ml/g of brain) was 0.0712 ± 0.0529 ml/min/g of brain, and it was significantly 40-fold greater than the CLin value and fully greater than the convective flow in ISF. Furthermore, no significant concentration gradient was observed between ISF and CSF. These results suggest that the CLout value mainly reflects the efflux clearance through the BBB. Additionally, the hippocampal ISF/plasma concentration ratio of baclofen was markedly increased by both systemic administration of probenecid and its direct instillation into ISF.
Conclusions. The restricted distribution of baclofen in the brain ISF may be ascribed to the efficient efflux from the brain through the BBB which is regulated possibly by a probenecid-sensitive organic anion transport system.
Similar content being viewed by others
REFERENCES
J.R. Bianchine. Drugs for Parkinson's disease, spasticity, and acute muscle spasms. In A.G. Gilman, L.S. Goodman, T.W. Rall, and F. Murad (ed.), The Pharmacological Basis of Therapeutics, 7th Ed, Macmillan Publishing Company, New York, 1985, pp. 473–490.
P.C. Waldmeier and P.A. Baumann. GABA B receptors and transmitter release. In N.G. Bowery, H. Bittiger, and H.T. Olpe (ed.), GABA B Receptors in Mammalian Function, John Wiley and Sons, New York, 1990, pp 63–80.
M.E. Otero and G.B. Acosta. Effects of baclofen on amino acid release. Eur. J. Pharmacol. 224: 21–25 (1992).
P.F. Morrison, P.M. Bungay, J.K. Hsiao, B.A. Ball, I.N. Mefford, and T.L. Dedrick. Quantitative microdialysis: Analysis of transients and application to pharmacokinetics in brain. J. Neurochem. 57: 103–119 (1991).
J.M. Collins and R.L. Dedrick. Distributed model for drug delivery to CSF and brain tissue. Am. J. Physiol. 245: R303–R310 (1983).
J.B.M.M. Bree, K.L. Audus, and R.T. Borchardt. Carrier-mediated transport of baclofen across monolayers of bovine brain endothelial cells in primary culture. Pharm. Res. 5: 369–371 (1988).
J.B.M.M. Bree, C.D. Heijligers-Feijen, A.G. Boer, M. Danhof, and D.D. Breimer. Stereoselective transport of baclofen across the blood-brain barrier in rats as determined by the unit impulse response methodology. Pharm. Res. 8: 259–262 (1991).
J.B. Justice, Jr. Quantitative microdialysis of neurotransmitters. J. Neurosci. Methods. 48: 263–276 (1993).
H. Benveniste and P.C. Huttemeier. Microdialysis—theory and application. Prog. Neurobiol. 35: 195–215 (1990).
T. Terasaki, Y. Deguchi, H. Sato, K. Hirai, and A. Tsuji. In vivo transport of a dynorphin-like analgesic peptide, E-2078, through the blood-brain barrier: An application of brain microdialysis. Pharm. Res. 8: 815–820 (1991).
T. Terasaki, Y. Deguchi, Y. Kasama, W.M. Pardridge, and A. Tsuji. Determination of in vivo steady-state unbound drug concentration in the brain ISF by microdialysis. Int. J. Pharm. 81: 143–152 (1992).
S.L. Wong, K. Belle, and R.J. Sawchuk. Distributional transport kinetics of zidovudine between plasma and brain extracellular fluid/cerebrospinal fluid in the rabbit; Investigation of the inhibitory effect of probenecid utilizing microdialysis. J. Pharmacol. Exp. Ther. 264: 899–909 (1993).
K.H. Dykstra, A. Arya, D.M. Arriola, P.M. Bungay, P.F. Morrison, and R.L. Dedrick. Microdialysis study of zidovudine (AZT) transport in rat brain. J. Pharmacol. Exp. Ther. 267: 1227–1236 (1993).
Y. Deguchi, T. Terasaki, S. Kawasaki, and A. Tsuji. Muscle microdialysis as a model study to relate the drug concentration in tissue interstitial fluid and dialysate. J. Pharmacobio-Dyn. 14: 483–492 (1991).
R.C. Chow and G. Levy. Effect of heparin or salicylate infusion on serum protein binding and on concentrations of phenytoin in serum, brain, and cerebrospinal fluid of rats. J. Pharmacol. Exp. Ther. 219: 42–48 (1981).
Y. Deguchi, T. Terasaki, H. Yamada, and A. Tsuji. An application of microdialysis to drug tissue distribution study: In vivo evidence for free-ligand hypothesis and tissue binding of β-lactam antibiotics in interstitial fluids. J. Pharmacobio-Dyn. 15: 79–89 (1992).
R.E. Galinsky, K.K. Flaharty, B.L. Hoesterey, and B.D. Anderson. Probenecid enhances central nervous system uptake of 2′,3′-dideoxyinosine by inhibiting cerebrospinal fluid efflux. J. Pharmacol. Exp. Ther. 257: 972–978 (1991).
R.G. Blasberg, J.D. Fenstermacher, and C.S. Patlak. Transport of α-aminoisobutyric acid across brain capillary and cellular membranes. J. Cereb. Blood Flow Metab. 3: 8–32 (1983).
O. Sakurada, C. Kennedy, J. Jehle, J.D. Brown, G.L. Carbin, and L. Sokoloff. Measurement of local cerebral blood flow with iodo [14C]antipyrine. Am. J. Physiol. 234: H59–H66 (1978).
K. Ohno, K.D. Pettigrew, and S.I. Rapoport. Lower limits of cerebrovascular permeability to nonelectrolytes in the conscious rat. Am. J. Physiol. 235: H299–H307 (1978).
R. Spector and A.V. Lorenzo. The effects of salicylate and probenecid on the cerebrospinal fluid transport of penicillin, aminosalicylic acid, and iodide. J. Pharmacol. Exp. Ther. 188: 55–65 (1974).
R. Spector. Ceftriaxone pharmacokinetics in the central nervous system. J. Pharmacol. Exp. Ther. 236: 380–383 (1985).
H. Suzuki, Y. Sawada, Y. Sugiyama, T. Iga, M. Hanano, and R. Spector. Transport of imipenem, a novel carbapenem antibiotics, in the rat central nervous system. J. Pharmacol. Exp. Ther. 250: 979–984 (1989).
M. Ogawa, H. Suzuki, Y. Sawada, M. Hanano, and Y. Sugiyama. Kinetics of active efflux via choroid plexus of β-lactam antibiotics from the CSF into the circulation. Am. J. Physiol. 266: R392–R399 (1994).
E.M. Cornford. The blood-brain barrier, A dynamic regulatory interface. Mol. Physiol. 7: 219–260 (1985).
E.M. Cornford, C.P. Diep, and W.M. Pardridge. Blood-brain barrier transport of valproic acid. J. Neurochem. 44: 1541–1550 (1985).
K.D.K. Adkison, A.A. Artru, K.M. Powers, and D.D. Shen. Contribution of probenecid-sensitive anion transport processes at the brain capillary endothelium and choroid plexus to the efficient efflux of valproic acid from the central nervous system. J. Pharmacol. Exp. Ther. 268: 797–805 (1994).
A. Tsuji, T. Terasaki, Y. Takabatake, Y. Tenda, I. Tamai, T. Yamashima, S. Moritani, T. Tsuruo, and J. Yamashita. Life Sci. 51: 1427–1437 (1992).
A. Sakata, I. Tamai, K. Kawazu, Y. Deguchi, T. Ohnishi, A. Saheki, and A. Tsuji. In vivo evidence for ATP-dependent and P-glycoprotein-mediated transport of cyclosporin A at the blood-brain barrier. Biochem. Pharmacol. 48: 1989–1992 (1994).
K. Yamaoka. MULTI2(BAYES). In R. Hori (ed.), Introduction to Population Pharmacokinetics, Yakugyo Giho Sha, Tokyo, 1988, pp 103–131 (in Japanese).
Rights and permissions
About this article
Cite this article
Deguchi, Y., Inabe, K., Tomiyasu, K. et al. Study on Brain Interstitial Fluid Distribution and Blood-Brain Barrier Transport of Baclofen in Rats by Microdialysis. Pharm Res 12, 1838–1844 (1995). https://doi.org/10.1023/A:1016263032765
Issue Date:
DOI: https://doi.org/10.1023/A:1016263032765