Abstract
Purpose
Nonsteroidal anti-inflammatory drugs (NSAIDs) often cause ulcers in the small intestine in humans, but there are few effective agents for treatment of small intestinal ulcers. We found that soluble dietary fibers (SDFs), such as pectin, could prevent the formation of small intestinal lesions induced by indomethacin (IND) in cats. To elucidate the mechanism of protection by SDFs, we examined the viscosities of SDFs and the effects of pectin on gastrointestinal absorption of IND and intestinal hypermotility induced by IND.
Methods
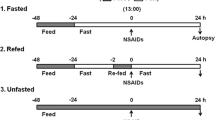
Cats were given regular dry food (RFD-Dry) or RFD-Dry supplemented with pectin, guar gum, polydextrose, or mucin twice daily. IND was administered orally once daily for 3 days. Mucosal lesions in the small intestine were examined 24 h after the final dosing of IND. Plasma concentrations of IND were measured by HPLC. GI motilities were measured using a telemetry system in conscious cats implanted with force transducers. Viscosities of the SDFs were measured using a viscosimeter.
Results
In cats given RFD-Dry, IND (3 mg/kg) increased motility and produced many lesions in the lower half of the small intestine; the total lesion area (TLA) was 7.5 ± 2.6 cm2 (n = 4). Lesions induced by IND were markedly decreased in cats given RFD-Dry supplemented with 3% pectin, guar gum, polydextrose or mucin; TLAs were 0.6 ± 0.3, 0.0 ± 0.0, 1.3 ± 0.8 and 1.6 ± 0.5 cm2 (n = 4) (P < 0.05 vs. RFD-Dry alone), respectively. The viscosity (mPa-S) of pectin, guar gum, polydextrose and mucin (3% concentration) was 414, >1,200, 1 and 4, respectively. Pectin did not affect the absorption of IND nor did it inhibit IND-induced intestinal hypermotility.
Conclusions
SDFs protect the small intestine against NSAID-induced damage, probably by compensating a barrier function of the mucin decreased by IND. Viscosities of the SDFs play a role, at least in part, in the protective effects of the SDFs on the small intestine.







Similar content being viewed by others
References
Chutkan R, Toubia N. Effect of nonsteroidal anti-inflammatory drugs on the gastrointestinal tract: diagnosis by wireless capsule endoscopy. Gastrointest Endosc Clin N Am. 2004;14:67–85.
Fortun PJ, Hawkey CJ. Nonsteroidal anti-inflammatory drugs and the small intestine. Curr Opin Gastroenterol. 2007;23:134–141.
Goldstein JL, Eisen GM, Lewis B, Gralnek IM, Zlotnick S, Fort JG. Video capsule endoscopy to prospectively assess small bowel injury with celecoxib, naproxen plus omeprazole, and placebo. Clin Gastroenterol Hepatol. 2005;3:133–141.
Laine L, Connors LG, Reicin A, et al. Serious lower gastrointestinal clinical events with nonselective NSAID or coxib use. Gastroenterology. 2003;124:288–292.
Maiden L, Thjodleifsson B, Theodors A, Gonzalez J, Bjarnason I. A quantitative analysis of NSAID-induced small bowel pathology by capsule enteroscopy. Gastroenterology. 2005;128:1172–1178.
Lanas Á, Scarpignato C. Microbial flora in NSAID-induced intestinal damage: a role for antibiotics? Digestion. 2006;73(suppl 1):136–150.
Wallace JL. Nonsteroidal anti-inflammatory drugs and gastroenteropathy: the second hundred years. Gastroenterology. 1997;112:1000–1016.
Whittle BRJ. Mechanisms underlying intestinal injury induced by anti- inflammatory COX inhibitors. Eur J Pharmacol. 2004;500:427–439.
Kunikata T, Tanaka A, Miyazawa T, Kato S, Takeuchi K. 16, 16-Dimethyl prostaglandin E2 inhibits indomethacin-induced small intestinal lesions through EP3 and EP4 receptors. Dig Dis Sci. 2002;47:894–904.
Anthony A, Pounder RE, Dhillon AP, Wakefield AJ. Vascular anatomy defines site of indomethacin induced jejunal ulceration along the mesenteric margin. Gut. 1997;41:763–770.
Miura S, Suematsu M, Tanaka S, et al. Microcirculatory disturbance in indomethacin-induced intestinal ulcer. Am J Physiol. 1991;261:G213–G219.
Asako H, Kubes P, Wallace J, Gaginella T, Wolf RE. Indomethacin-induced leukocyte adhesion in mesenteric venules: role of lipoxygenase products. Am J Physiol. 1992;262:G903–G908.
Robert A, Asano T. Resistance of germfree rats to indomethacin-induced intestinal lesions. Prostaglandins. 1977;14:333–341.
Satoh H, Guth PH, Grossman MI. Role of food in gastrointestinal ulceration produced by indomethacin in the rat. Gastroenterology. 1982;83:210–215.
Ishihara Y, Okabe S. Effects of cholestyramine and synthetic hydrotalcite on acute gastric or intestinal lesion formation in rats and dogs. Dig Dis Sci. 1981;26:553–560.
Satoh H, Guth PH, Grossman MI. Role of bacteria in gastric ulceration produced by indomethacin in the rat: cytoprotective action of antibiotics. Gastroenterology. 1983;84:483–489.
Takeuchi K, Miyazawa T, Tanaka A, Kato S, Kunikata T. Pathogenic importance of intestinal hypermotility in NSAID-induced small intestinal damage in rats. Digestion. 2002;66:30–41.
Tanaka A, Matsumoto M, Hayashi Y, Takeuchi K. Functional mechanism underlying cycloxygenase-2 expression in rat small intestine following administration of indomethacin: relation to intestinal hypermotility. J Gastroenterol Hepatol. 2005;20:38–45.
Satoh H, Shiotani S, Otsuka N, Hato K, Nishimura S. Role of dietary fibers, intestinal hypermotility and leukotrienes in the pathogenesis of NSAID-induced small intestinal ulcers in cats. Gut (in press).
Bueno L, Praddaude F, Fioramonti J, Ruckebusch Y. Effect of dietary fiber on gastrointestinal motility and jejunal transit time in dogs. Gastroenterology. 1981;80:701–707.
Xu X, Brining D, Rafiq A, Hayes J, Chen J. Effects of enhanced viscosity on canine gastric and intestinal motility. J Gastroenterol Hepatol. 2005;20:387–394.
Ebihara K, Maduhara R, Kiriyama S. Major determinants of plasma glucose-flattening activity of a water-soluble dietary fiber: effects of Konjak mannan on gastric emptying and intraluminal glucose-diffusion. Nutr Rep Int. 1981;23:1145–1156.
Jenkins DJA, Wolever TMS, Leeds AR, et al. Dietary fibres, fibre analogues, and glucose tolerance: importance of viscosity. Br Med J. 1978;1:1392–1394.
Reuter BK, Davies NM, Wallace JL. Nonsteroidal anti-inflammatory drug enteropathy in rats: role of permeability, bacteria, and enterohepatic circulation. Gastroenterology. 1997;112:109–117.
Shimoyama Y, Kusano M, Kawamura O, et al. High-viscosity liquid meal accelerates gastric emptying. Neurogastroenterol Motil. 2007;19:879–886.
Cherbut C, Albina E, Champ M, Doublier JL, Lecannu G. Action of guar gum on the viscosity of digestive contents and on the gastrointestinal motor function in pigs. Digestion. 1990;46:205–213.
Schönfeld JV, Evans DF, Wingate DL. Effect of viscous fiber (guar) on postprandial motor activity in human small bowel. Dig Dis Sci. 1997;42:1613–1617.
Acknowledgments
The authors wish to thank Dr. M. Morimoto of Research Center for Bioscience and Technology, Tottori University, and Dr. S. Nakamura of Research Division, Ophtecs, Japan, for their useful advices on the viscosity studies and pharmacokinetic studies. We are greatly indebted to Dr. Y. Akiba (CURE/UCLA & BBRI, Los Angeles, California) for providing valuable discussion and suggestions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Satoh, H., Hara, T., Murakawa, D. et al. Soluble Dietary Fiber Protects Against Nonsteroidal Anti-inflammatory Drug-Induced Damage to the Small Intestine in Cats. Dig Dis Sci 55, 1264–1271 (2010). https://doi.org/10.1007/s10620-009-0893-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-009-0893-2