Abstract
Rationale
Schizophrenia is a disorder with cognitive deficits that could stem from cholinergic dysfunction.
Objectives
Our aim was to examine if donepezil administered to stable, medicated outpatients with schizophrenia improves cognition and psychopathology.
Methods
We conducted a double-blind placebo-controlled trial of donepezil up to 10 mg/day added for 8 weeks to ongoing antipsychotic treatment in 36 typical community-treated schizophrenia patients not selected for cognitive impairment.
Results
Donepezil did not improve measures of cognition or psychopathology. It was well tolerated.
Conclusion
Consistent with other studies, addition of donepezil to stable patients with schizophrenia did not improve cognition or measures of psychopathology. This result does not support the hypothesis that residual symptoms and cognitive problems result from a cholinergic deficit that can be remedied by an acetylcholinesterase inhibitor. A donepezil add-on strategy might make sense in selected schizophrenia cases where a pathological process is known to affect cholinergic neurons (e.g., history of head injury or comorbid dementia).
Similar content being viewed by others
Introduction
Can we view schizophrenia as a disorder with a cholinergic deficit? A large body of evidence in animals and humans has established that the cholinergic neurotransmitter system is important for attention, memory, and learning, involving both the nicotinic and muscarinic systems (Friedman 2004; Furey et al. 2000; Hasselmo and Bower 1993). In schizophrenia, patients often show cognitive deficits in these areas, particularly in learning and verbal memory (Green 1996). A cholinergic deficit can theoretically stem from insufficient output of acetylcholine, e.g., from gross destruction of cholinergic neurons as it occurs in dementia of the Alzheimer type (DAT) (Arendt et al. 1983); from reduction in the activity of the enzyme, choline acetyltransferase (CAT), which synthesizes acetylcholine; or from insufficient action at the target receptors. Some authors have pointed out that schizophrenia and DAT share some clinical characteristics beyond cognitive problems, including psychosis and negative symptoms (Reichman et al. 1996; White and Cummings 1996). However, neuropathological studies clearly refute that schizophrenia is a disorder of too few cholinergic neurons (el-Mallakh et al. 1991) or of decreased synthetic capacity of cholinergic neuron populations (Powchik et al. 1998). Rather, in schizophrenia the dysfunction seems to be located at the cholinergic receptor level of both nicotinic and muscarinic subtypes. Direct evidence of involvement of muscarinic receptors in schizophrenia comes from postmortem work showing decreased mRNA of M1 receptors (Dean et al. 2002) and a SPECT imaging study showing decreased availability of muscarinic receptors (Raedler et al. 2003). Nicotinic receptors, including the low-affinity alpha7 receptor subtype, are reduced in the hippocampus of patients with schizophrenia (Freedman et al. 1995). This receptor subtype is involved in sensory gating, a hippocampal neurophysiological phenomenon that is typically impaired in patients with schizophrenia (Adler et al. 1993). The alpha7 receptor is of particular interest because the region on chromosome 15 that contains the gene for this receptor subtype has been linked to schizophrenia (Freedman et al. 1997). Pharmacological trials in unmedicated patients with schizophrenia have shown an improvement in negative symptoms with anticholinergic treatment (Tandon 1999; Tandon and Greden 1989). This, however, has not been found in all trials (Goff et al. 1994).
Indirect evidence includes the high rates of cigarette smoking in patients with schizophrenia (Goff et al. 1992; McEvoy and Allen 2003) and findings of cognitive and symptomatic benefit from nicotine (Dalack et al. 1998) and from the muscarinic agonist, betel nut (Sullivan et al. 2000). Betel nut contains a direct muscarinic agonist, arecoline; similar direct muscarinic agonists are currently under development but not yet available for clinical use. One such drug, xanomeline, shows a gene expression profile similar to atypical antipsychotics (Perry et al. 2001).
Taken together, some manifestations of schizophrenia could be the result of an overall cholinergic deficit. Enhancing the availability of acetylcholine at the synaptic cleft by inhibiting its metabolizing enzyme, acetylcholinesterase (AChE) might therefore ameliorate some problems that are due to hypofunction of nicotinic and/or muscarinic receptors. However, until donepezil, a well-tolerated, oral inhibitor of AchE, became available for clinical use it was difficult to increase cholinergic tone in the central nervous system. Donepezil is a competitive, reversible inhibitor of AChE that is approved in the United States for the treatment of dementia of the Alzheimer type and is, at least for this indication, well tolerated. It is effective not only for the cognitive manifestations of the dementing process but also for the frequent comorbid psychosis and behavioral problems (Wynn and Cummings 2004), consistent with a role of the cholinergic system in psychosis.
We located two randomized, double-blind trials in which donepezil was used as an add-on agent to stable schizophrenia patients maintained on their antipsychotic medication (Friedman et al. 2002; Tual et al. 2004). Both trials were negative: donepezil had no effect on measures of cognition or psychopathology. One trial used a crossover design of only 12 patients and might thus have been insufficiently powered to detect even a large effect size (Tual et al. 2004). Friedman et al. (2002) studied 36 patients in a parallel group design in which patients were randomized to placebo or donepezil, either 5 or 10 mg; thus, not all patients received the highest approved dose of donepezil. Patients for this trial were selected if they showed cognitive impairment, defined as scoring two standard deviations below the norm for the California Verbal Learning Test (CVLT), a test of secondary memory.
We conducted a double-blind, placebo-controlled trial in which we added a full therapeutic dose of donepezil to representative community patients with schizophrenia not selected for the presence of cognitive impairment. We hypothesized that some aspects of impaired cognition are mediated by a cholinergic deficit in schizophrenia that might be ameliorated by donepezil. We also examined the effects of cholinergic manipulation on psychosis and general psychopathology.
Materials and methods
Study setting and sponsorship
The study was conducted at two sites: an urban mental health center in downtown Boston (the Freedom Trail Clinic at the Erich Lindemann Mental Health Center), and a VA outpatient clinic just outside of Metro Boston (the Edith Nourse Rogers Memorial VA Hospital). The study was sponsored by Pfizer Inc. in the form of an investigator-initiated unrestricted grant.
Patient selection
Subjects were referred for this study by their clinicians. The research team assessed competency to participate in clinical research with a semistructured interview (available upon request). All subjects consented in writing to participate in this trial. The study was approved by the responsible institutional review boards.
Characteristics of subjects
Subjects had to have schizophrenia as their primary diagnosis, and they had to be deemed psychiatrically stable on an antipsychotic medication. Diagnoses were based on physician interview and chart review (O.F. and L.H.), using DSM-IV criteria (American Psychiatric Association Committee on Nomenclature and Statistics 1994). Subjects were excluded if there was an active substance use disorder within the past 3 months, not counting nicotine dependence. Subjects were also excluded if they had any cognitive disorder (including mental retardation) or developmental disorder as determined by chart review or if they scored less than 20 on the Mini-Mental State Examination (MMSE) (Folstein et al. 1975). Subjects taking antipsychotics that are considered strongly anticholinergic were excluded (e.g., clozapine and low-potency conventional antipsychotics); subjects could not be on ancillary medications with anticholinergic properties (e.g., benztropine or trihexyphenidyl).
Study design and procedures
This was a parallel-group, placebo-controlled, double-blind trial in which subjects received either donepezil or placebo for 8 weeks. Study medication was added to the subject’s stable antipsychotic regimen. Subjects were assessed with standard rating scales of psychopathology at baseline, after 2, 4, and 8 weeks. Side effects and adverse events were assessed every 2 weeks. Cognition was measured by a cognitive battery at baseline and after 8 weeks.
Drug regimen
Subjects started with a 5-mg daily dose of donepezil. After 4 weeks, the dose was increased to 10 mg daily for another 4 weeks. Donepezil and placebo were prepared in identical-appearing capsules, which were dispensed every 2 weeks; surplus capsules were counted each study visit. All subjects remained on their stable antipsychotic during the trial.
Ratings
Clinical psychopathology was assessed with standard ratings scales for schizophrenia: the Positive and Negative Syndrome Scale (PANSS) (Kay et al. 1987) for summary ratings supplemented by the Scale for the Assessment of Negative Symptoms (SANS) (Andreasen 1982, 1983) for negative symptoms and the Calgary Depression Scale for Schizophrenia (CDSS) (Addington et al. 1990), a rating scale specifically designed to rate depression in patients with schizophrenia. We measured side effects with the Simpson–Angus Rating Scale (SARS, CATIE-modified version) (Simpson and Angus 1970), the Barnes Akathisia Rating Scale (BARS) (Barnes 1989), and the Abnormal Involuntary Movement Scale (AIMS) (Guy 1976). Adverse effects were collected with the Systematic Assessment for Treatment Emergent Events (SAFTEE) (Levine and Schooler 1986), a rating scale that contains both open-ended and closed inquiries.
A cognitive battery comprised of standard items used in schizophrenia research and selected for domains usually affected in schizophrenia and possibly sensitive to procholinergic agents was used. Cognitive domains probed were attention and short-term memory, verbal learning, set-shifting abilities, verbal fluency, and visuospatial function and motor speed. Attention and short-term memory were assessed using the Digit Span subtest from the Wechsler Memory Scale (WAIS-III) (Wechsler 1997); verbal learning was assessed by the three learning trials of the Hopkins Verbal Learning Test—Revised (HVLT-R) (Benedict et al. 1998); set-shifting abilities were assessed using the Trail Making Test, parts A and B (Trail A and B) (Spreen and Strauss 1991); word fluency was assessed using the Benton Oral Word Association Test (Benton and Hamsher 1978); and visuomotor function and motor speed were assessed using the Grooved Pegboard Test (model 32025, Lafayette Instrument Company).
Data analysis
Clinical variables were analyzed using repeated measures analysis of variance (ANOVA) with group (drug vs placebo) as the between-subjects factor and time (baseline, week 2, week 4, and week 8) as the within-subjects factor. For missing data, the last observation was carried forward (LOCF analysis). The cognitive variables were analyzed using mixed-model ANOVA with group (drug vs placebo) as the between-subjects factor and time (pretreatment vs posttreatment) as the within-subjects factor, with IQ included as a covariate followed by simple F tests. Baseline comparisons were made with t tests or chi-square analysis, depending on the nature of the respective variable. All tests were two-tailed, with level of significance set at 0.05.
Results
Subject details
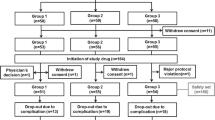
Forty subjects agreed to participate; 4 subjects withdrew consent after randomization before they received any study medication. The remaining 36 subjects compose the sample for this study. Of the 36 subjects, 19 were randomized to active study medication and 17 to placebo. Four subjects did not finish the 8-week trial, leaving 32 study completers. Complete cognitive data were available for 30 subjects.
The demographic characteristics and baseline measures of our study sample were as follows: most subjects were male (91.7%), white (88.9%), and smoked (80%). Only three subjects in the placebo group and four patients in the donepezil group did not smoke. The average age of subjects was 48.7 years (range, 24–64 years). Most had never married (72.2%), and they had an education of 12.2 years (compared to 13.3 years parental education). The estimated IQ based on NAART scores (Blair and Spreen 1989; Spreen and Strauss 1991) was 96.2 (range, 74.4–118.0). Mean MMSE score was 27.3 (range, 21–30). On average, subjects were first hospitalized at age 23 (range, 13–41 years), with an average duration of illness of 25 years (range, 1–43 years). Among the subjects, 66.7% of the sample had been hospitalized more than four times over their lives. PANSS total score was 64.6 (range, 44–96), SANS total score was 48.5 (range, 14–80), indicating generally mild psychopathology. The only significantly different baseline variable between the groups was the estimated IQ (103 in the placebo group, 90 in the donepezil group; F=13.5, df 1, p=0.001).
The most commonly used antipsychotic was olanzapine (13 subjects or 36%), followed by risperidone (10 patients or 28%). Olanzapine and risperidone were about evenly distributed in the placebo and donepezil group. Other antipsychotics were distributed between aripiprazole, fluphenazine, haloperidol, quetiapine, and ziprasidone; five patients received a combination of two antipsychotics.
Compliance as judged by pill count of returned medicines every visit was excellent, with most patients missing no pills at all. Only for three study visits was compliance estimated as partial (defined as less than 80% of pills taken).
Measures of psychopathology and side effects
Clinical ratings at baseline, after 4 weeks of treatment, and after 8 weeks of treatment remained essentially unchanged (table of mean values and standard deviation of clinical ratings available upon request). Repeated measures analysis showed no main effect of time or drug, or of time by drug interaction (data not shown). There was thus no benefit of medications on any measure of psychopathology and no improvement or worsening of side effects.
Cognitive measures
Table 1 shows the results of the cognitive tests for both subject groups pre- and posttreatment with calculated effect sizes. There were no statistically significant differences between groups on any of the cognitive measures by mixed-model ANOVA (data not shown). We would have needed 35 subjects in each group to have 80% statistical power to detect an effect of Cohen’s d=0.6 with an α=0.05; the only measure in our battery with that large of an effect size was the Trail Making Test, part A.
Even though we did not select for cognitive impairment, our study sample of chronic patients showed typical and expected poor performance on the cognitive tests; generally, subjects scored between one and two standard deviations below the norms for normal controls.
Safety and tolerability
Donepezil was well tolerated. Only one donepezil subject did not complete the study because of an intercurrent medical illness in need of hospitalization, which was not attributable to donepezil. There were two serious adverse events, both in subjects assigned to donepezil; neither was attributed to donepezil. Treatment-emergent or worsening side effects as collected with the SAFTEE and analyzed according to expectable donepezil side effects (from larger samples (Dunn et al. 2000; Mohs et al. 2001)) were rare and not significantly different between the treatment and placebo group. Possible donepezil side effects that we examined were asthenia, headache, sialorrhea, diarrhea, dyspepsia, nausea/vomiting, insomnia, agitation, dizziness, abnormal dreams, rhinitis, and micturition problems. We noticed sialorrhea in three donepezil subjects and in no placebo patient; sialorrhea is not usually listed as a common problem (but biologically plausible). Adding donepezil did not change ratings of extrapyramidal symptoms, akathisia, or tardive dyskinesia (TD). Seven subjects, four of whom received donepezil, had AIMS scores of at least 4 at baseline. Although AIMS ratings improved from 5.75 to 3.75 (SD 3.742) in these donepezil subjects, this was not significant by t test (t=1.1; p=0.363).
Discussion
This was a negative trial: patients with schizophrenia who received donepezil added to their maintenance antipsychotic did not improve on measures of psychopathology or cognition. Donepezil was well tolerated. Whereas some uncontrolled trials suggest efficacy of this add-on strategy, our trial is consistent with the negative results of the other two double-blind trials that used donepezil as the augmenting medication.
What could account for our negative findings? Clearly, our trial was only powered to detect larger effects that we would consider to be clinically meaningful. Our trial was not powered to detect small or medium effect sizes, which might be more realistic to expect judging from trials of donepezil in DAT. While not directly comparable, improvement in Alzheimer’s disease has been estimated to average 0.8 points on the MMSE (95% confidence interval, 0.5–1.2) with donepezil treatment (AD 2000 Collaborative Group 2004); this is a small improvement in cognition of dubious clinical significance. It is possible that we selected the wrong tests to sample effects of cholinergic function, but for pragmatic and statistical reasons we thought it would be important to limit the number of outcome measures. Nevertheless, we would have expected some signal in one of the tests if donepezil were effective. Our trial lasted only 8 weeks and might be too short.
Next, we could have studied the wrong patient population. For one, our sample of chronic, disabled patients may be particularly refractory to the intervention. Furthermore, we excluded patients with a history of traumatic brain injury (TBI). TBI has clear deleterious effects on cholinergic neurons, and donepezil is a reasonable strategy that can be tried (Arciniegas 2003; Griffin et al. 2003). Similarly, elderly schizophrenic patients with comorbid dementia would be another patient group where procholinergic agents would be a rational choice. Patients with TD might be yet another group of patients where there is some support for using donepezil (Caroff et al. 2001). The few patients in our cohort with TD did not respond, however.
Smoking is perhaps the biggest confounder, at least for any remedial role of donepezil for the nicotinic arm of the cholinergic system. One can theorize that patients are already treating their putative cholinergic dysfunction maximally with nicotine. On the other hand, nicotinic neurons desensitize quickly when exposed to nicotine. Donepezil is a rather blunt instrument that floods the brain with acetylcholine. This can have effects of adaptation in different brain areas, including leading to desensitization of nicotinic receptors in the hippocampus, which renders the additional acetylcholine made available by donepezil useless. Even in nonsmokers, daily dosing of a procholinergic agent might not be the best strategy. It is hard of course to argue for an intervention that has as its prerequisite the lack of a behavior in the target population that most display (smoking). The patients that we studied (most of whom smoked) constitute the bulk of patients with schizophrenia. Therefore, donepezil use would be limited to the approximately 20% of patients who do not smoke.
To get around adaptation, pharmacological principles beyond AChE inhibition might be necessary (Maelicke and Albuquerque 2000). This is suggested by a successful trial of galantamine in schizophrenia, which, in addition to blocking AchE, allosterically modulates nicotinic receptors, thereby preventing nicotinic receptor desensitization (Allen et al. 2003). In this double-blind, placebo-controlled trial, galantamine improved a measure of attention and verbal fluency.
In summary, the results of this and two other double-blind, placebo-controlled trials do not support the addition of donepezil to stable patients with schizophrenia for improvement of cognition or psychopathology. The residual symptoms and cognitive problems do not appear to result from a cholinergic deficit that can be easily remedied by a nonspecific AChE inhibitor. It could also be that schizophrenia sensu strictu is not a disorder of cholinergic deficit at all. However, ours was a pragmatic trial of established and medicated patients, not a proof-of-concept study where unmedicated, nonrefractory patients would be more appropriate. Our study thus does not rule out a more subtle and more complicated role of the cholinergic system in schizophrenia, such as a very selective and relatively small loss of only certain cholinergic neuron populations (Holt et al. 1999). A donepezil add-on strategy makes sense in those selected cases where a pathological process is known to affect cholinergic neurons (e.g., history of head injury or comorbid dementia). The value of donepezil in first-episode patients (who are presumably not refractory), particularly if they are nonsmokers, remains to be studied. Future trials might also go beyond acute symptoms and instead focus on long-term neuroprotective effects of agents like donepezil (Takada et al. 2003). It is discouraging, however, that even in disorders with well-defined cholinergic pathology (i.e., DAT) it has been very difficult to show clear-cut clinical benefit (AD 2000 Collaborative Group 2004).
References
AD 2000 Collaborative Group (2004) Long-term donepezil treatment in 565 patients with Alzheimer’s disease (AD 2000): randomised double-blind trial. Lancet 363:2105–2115
Addington D, Addington J, Schissel B (1990) A depression rating scale for schizophrenia. Schizophr Res 3:247–251
Adler LE, Hoffer LD, Wiser A, Freedman R (1993) Normalization of auditory physiology by cigarette smoking in schizophrenic patients. Am J Psychiatry 150:1856–1861
Allen T, McEvoy JP, Keefe R, Levin E, Wilson W (2003) Galantamine as an adjunctive therapy in the treatment of schizophrenia. In: 11th Congress of the International Psychogeriatric Association (IPA), Chicago, 17–22
American Psychiatric Association Committee on Nomenclature and Statistics (1994) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Washington, DC
Andreasen NC (1982) Negative symptoms in schizophrenia: definition and reliability. Arch Gen Psychiatry 39:784–788
Andreasen NC (1983) Scale for the Assessment of Negative Symptoms (SANS). University of Iowa, Iowa City
Arciniegas DB (2003) The cholinergic hypothesis of cognitive impairment caused by traumatic brain injury. Curr Psychiatr Rep 5:391–399
Arendt T, Bigl V, Arendt A, Tennstedt A (1983) Loss of neurons in the nucleus basalis of Meynert in Alzheimer’s disease, paralysis agitans and Korsakoff’s disease. Acta Neuropathol (Berl) 61:101–108
Barnes TRE (1989) A rating scale for drug-induced akathisia. Br J Psychiatry 154:672–676
Benedict RHB, Schretlen D, Groninger L, Brandt J (1998) The Hopkins verbal learning test—revised. Clin Neuropsychol 12:43–55
Benton A, Hamsher K (1978) Multilingual aphasia examination (manual revised). University of Iowa, Iowa City
Blair J, Spreen O (1989) Predicting premorbid IQ: a revision of the national adult reading test. Clin Neuropsychol 3:129–136
Caroff SN, Campbell EC, Havey J, Sullivan KA, Mann SC, Gallop R (2001) Treatment of tardive dyskinesia with donepezil: a pilot study. J Clin Psychiatry 62:772–775
Dalack GW, Healey DJ, Meador-Woodruff JH (1998) Nicotine dependence in schizophrenia: clinical phenomena and laboratory findings. Am J Psychiatry 155:1490–1501
Dean B, McLeod M, Keriakous D, McKenzie J, Scarr E (2002) Decreased muscarinic1 receptors in the dorsolateral prefrontal cortex of subjects with schizophrenia. Mol Psychiatry 7:1083–1091
Dunn NR, Pearce GL, Shakir SAW (2000) Adverse effects associated with the use of donepezil in general practice in England. J Psychopharmacol 14:406–408
el-Mallakh RS, Kirch DG, Shelton R, Fan KJ, Pezeshkpour G, Kanhouwa S, Wyatt RJ, Kleinman JE (1991) The nucleus basalis of Meynert, senile plaques, and intellectual impairment in schizophrenia. J Neuropsychiatry Clin Neurosci 3:383–386
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Freedman R, Hall M, Adler LE, Leonard S (1995) Evidence in postmortem brain tissue for decreased numbers of hippocampal nicotinic receptors in schizophrenia. Biol Psychiatry 38:22–33
Freedman R, Coon H, Myles-Worsley M, Orr-Urtreger A, Olincy A, Davis A, Polymeropoulos M, Holik J, Hopkins J, Hoff M, Rosenthal J, Waldo MC, Reimherr F, Wender P, Yaw J, Young DA, Breese CR, Adams C, Patterson D, Adler LE, Kruglyak L, Leonhard S, Byerley W (1997) Linkage of a neurophysiological deficit in schizophrenia to a chromosome 15 locus. Proc Natl Acad Sci U S A 94:587–592
Friedman JI (2004) Cholinergic targets for cognitive enhancement in schizophrenia: focus on cholinesterase inhibitors and muscarinic agonists. Psychopharmacology 174:45–53
Friedman JI, Adler DN, Howanitz E, Harvey PD, Brenner G, Temporini H, White L, Parrella M, Davis KL (2002) A double blind placebo controlled trial of donepezil adjunctive treatment to risperidone for the cognitive impairment of schizophrenia. Biol Psychiatry 51:349–357
Furey ML, Pietrini P, Haxby JV (2000) Cholinergic enhancement and increased selectivity of perceptual processing during working memory. Science 290:2315–2319
Goff DC, Henderson DC, Amico E (1992) Cigarette smoking in schizophrenia: relationship to psychopathology and medication side effects. Am J Psychiatry 149:1189–1194
Goff DC, Amico E, Dreyfuss D, Ciraulo DA (1994) A placebo-controlled trial of trihexyphenidyl in unmedicated patients with schizophrenia. Am J Psychiatry 151:429–432
Green MF (1996) What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 153:321–330
Griffin SL, van Reekum R, Masanic C (2003) A review of cholinergic agents in the treatment of neurobehavioral deficits following traumatic brain injury. J Neuropsychiatry Clin Neurosci 15:17–26
Guy W (1976) ECDEU Assessment manual for psychopharmacology—revised (DHEW Publ No ADM 76-338). U.S. Department of Health, Education and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, NIMH Psychopharmacology Research Branch, Division of Extramural Research Programs
Hasselmo ME, Bower JM (1993) Acetylcholine and memory. Trends Neurosci 16:218–222
Holt DJ, Herman MM, Hyde TM, Kleinman JE, Sinton CM, German DC, Hersh LB, Graybiel AM, Saper CB (1999) Evidence for a deficit in cholinergic interneurons in the striatum in schizophrenia. Neuroscience 94:21–31
Kay SR, Fiszbein A, Opler LA (1987) The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 13:261–276
Levine J, Schooler NR (1986) SAFTEE: a technique for the systematic assessment of side effects in clinical trials. Psychopharmacol Bull 22:343–381
Maelicke A, Albuquerque EX (2000) Allosteric modulation of nicotinic acetylcholine receptors as a treatment strategy for Alzheimer’s disease. Eur J Pharmacol 393:165–170
McEvoy JP, Allen TB (2003) Substance abuse (including nicotine) in schizophrenic patients. Curr Opin Psychiatry 16:199–205
Mohs RC, Doody RS, Morris JC, Ieni JR, Rogers SL, Perdomo CA, Pratt RD, “312” Study Group (2001) A 1-year, placebo-controlled preservation of function survival study of donepezil in AD patients. Neurology 57:481–488
Perry KW, Nisenbaum LK, George CA, Shannon HE, Felder CC, Bymaster FP (2001) The muscarinic agonist xanomeline increases monoamine release and immediate early gene expression in the rat prefrontal cortex. Biol Psychiatry 49:716–725
Powchik P, Davidson M, Haroutunian V, Gabriel SM, Purohit DP, Perl DP, Harvey PD, Davis KL (1998) Postmortem studies in schizophrenia. Schizophr Bull 24:325–341
Raedler TJ, Knable MB, Jones DW, Urbina RA, Gorey JG, Lee KS, Egan MF, Coppola R, Weinberger DR (2003) In vivo determination of muscarinic acetylcholine receptor availability in schizophrenia. Am J Psychiatry 160:118–127
Reichman WE, Coyne AC, Amirneni S, Molino B, Egan S (1996) Negative symptoms in Alzheimer’s disease. Am J Psychiatry 153:424–426
Simpson GM, Angus JWS (1970) A rating scale for extrapyramidal side effects. Acta Psychiatr Scand 212:11–19
Spreen O, Strauss E (1991) A compendium of neuropsychological tests. Oxford University Press, New York
Sullivan RJ, Allen JS, Otto C, Tiobech J, Nero K (2000) Effects of chewing betel nut (Areca catechu) on the symptoms of people with schizophrenia in Palau, Micronesia. Br J Psychiatry 177:174–178
Takada Y, Yonezawa A, Kume T, Katsuki H, Kaneko S, Sugimoto H, Akaike A (2003) Nicotinic acetylcholine receptor-mediated neuroprotection by donepezil against glutamate neurotoxicity in rat cortical neurons. J Pharmacol Exp Ther 306:772–777
Tandon R (1999) Cholinergic aspects of schizophrenia. Br J Psychiatry 174(Suppl 37):7–11
Tandon R, Greden JF (1989) Cholinergic hyperactivity and negative schizophrenic symptoms. A model of cholinergic/dopaminergic interactions in schizophrenia. Arch Gen Psychiatry 46:745–753
Tual N, Yazc KM, Yacolu AE, Gogus A (2004) A double-blind, placebo controlled, cross-over trial of adjunctive donepezil for cognitive impairment in schizophrenia. Int J Neuropsychopharmacol 7:117–123
Wechsler D (1997) Wechsler Adult Intelligence Scale, 3rd edn. (WAIS-III). The Psychological Corporation, San Antonio, TX
White KE, Cummings JL (1996) Schizophrenia and Alzheimer’s disease: clinical and pathophysiologic analogies. Compr Psychiatry 37:188–195
Wynn ZJ, Cummings JL (2004) Cholinesterase inhibitor therapies and neuropsychiatric manifestations of Alzheimer’s disease. Dement Geriatr Cogn Disord 17:100–108
Acknowledgements
Funding for this trial was provided by an investigator-investigated grant from Pfizer, Inc (Oliver Freudenreich). This research was further supported by the National Alliance for Research in Schizophrenia and Depression (NARSAD) and the Clinical Research and Training Fellowship (CRTF) (Thilo Deckersbach) and K24 MH0205 (Donald C. Goff).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Freudenreich, O., Herz, L., Deckersbach, T. et al. Added donepezil for stable schizophrenia: a double-blind, placebo-controlled trial. Psychopharmacology 181, 358–363 (2005). https://doi.org/10.1007/s00213-005-2235-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-005-2235-1