Abstract
Purpose
Propofol is thought to act on γ-aminobutyric acid receptors, which have some role in pain transmission in the spinal cord. In this study, we examined the effects of intrathecal propofol on acute thermallyor inflammation-induced pain in rats.
Methods
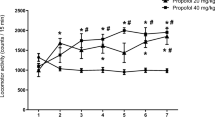
Lumbar intrathecal catheters were implanted in Male Sprague-Dawley rats. The tail withdrawal response to thermal stimulation (tail flick test) or paw flinching and shaking response bysc formalin injection into the hind paw (formalin test) were tested. Propofol 1000, 300 or 100μg or saline (control) was administered as 10 μL intrathecally. Motor disturbance and behavioural side effects were also monitored in the rats during the tail flick test. Eight rats were used for each dose in each test.
Results
No analgesic effects were observed in the tail flick test. In the formalin test, 50% of effective doses were 449 μg (95% confidence interval, 80–3180 μg) in phase 1 and 275 μg (146–519 μg) in phase 2. Motor disturbance was observed in one rat with 100μg and agitation and allodynia were seen in one rat with 300μg. However, both were reversible in 120 min.
Conclusions
Intrathecal administration of propofol had analgesic effects on inflammation-induced acute and facilitated pain but not on thermally-induced acute pain. Transient motor and sensory disturbance could not rule out the possibility of neurotoxicity.
Résumé
Objectif
On croit que le propofol agit sur les récepteurs de l’acide γaminobutyrique, lesquels jouent un certain rôle dans la transmission de la douleur dans la moelle épinière. Nous avons vérifié les effets du propofol intrathécal sur la douleur aiguë induite par la chaleur ou l’inflammation chez les rats.
Méthode
Des cathéters lombaires intrathécaux ont été implantés chez des rats mâles Sprague-Dawley. La réaction à la stimulation thermale par le retrait de la queue (test de latence de rétraction de la queue) ou le tressaillement de la patte et les secousses provoquées par l’injection sc de formol dans la patte arrière (test au formol) ont été analysés. Des doses intrathécales de 1 000, 300 ou 100 μg de propofol ou une solution saline (témoin) ont été administrées en 10 μL. Les troubles moteurs et les effets secondaires comportementaux ont aussi été enregistrés pendant le test de latence de rétraction de la queue. Huit rats ont été utilisés pour chaque dose de chaque test.
Résultats
Aucun effet analgésique n’a été observé pendant le test de latence de rétraction de la queue. Lors du test au formol, 50 % des doses efficaces ont été de 449 μg (intervalle de confiance de 95 %, 80– 3180 μg) pendant la phase 1 et de 275 μg (146– 519 μg) pendant la phase 2. Des troubles moteurs ont été observés chez un rat avec 100 μg et de l’agitation et de l’allodynie chez un rat avec 300 μg. Cependant, les deux réactions se sont renversées en 120 min.
Conclusion
L’administration intrathécale de propofol a des effets analgésiques sur la douleur aiguë induite et facilitée par l’inflammation, mais non sur la douleur aiguë induite par la chaleur. La présence de troubles moteurs et sensitifs transitoires n’exclut pas la possibilité de neurotoxicité.
Similar content being viewed by others
References
Hales T, Lambert JJ. The actions of propofol on inhibitory amino acid receptors of bovine adrenomedullary chromaffin cells and rodent central neurones. Br J Pharmacol 1991; 104: 619–28.
Ratnakumari L, Hemmings HC Jr. Effects of propofol on sodium channel-dependent sodium influx and glutamate release in rat cerebrocortical synaptosomes. Anesthesiology 1997; 86: 428–39.
Patel S, Wohlfeil ER, Rademacher DJ, et al. The general anesthetic propofol increases brain N-arachidonylethanolamine (anandamide) content and inhibits fatty acid amide hydrolase. Br J Pharmacol 2003; 139: 1005–13.
Millan MJ. The induction of pain: an integrative review. Prog Neurobiol 1999; 57: 1–164.
Xu TL. γ-aminobutyric acid-induced responses in acutely dissociated neurons from the rat sacral dorsal commissural nucleus. J Auton Nerv Syst 1999; 75: 156–63.
Dong XP, Xu TL. The actions of propofol on γ-aminobutyric acid-A and glycine receptors in acutely dissociated spinal dorsal horn neurons of the rat. Anesth Analg 2002; 95: 907–14.
Shimizu M, Yamakura T, Tobita T, et al. Propofol enhances GABAA receptor-mediated presynaptic inhibition in human spinal cord. Neuroreport 2002; 13: 357–60.
Anker-Moller E, Spangsberg N, Arendt-Nielsen L, Schultz P, Kristensen MS, Bjerring P. Subhypnotic doses of thiopentone and propofol cause analgesia to experimentally induced acute pain. Br J Anaesth 1991; 66: 185–8.
Erenmemisoglu A, Madenoglu H, Tekol Y. Antinociceptive effect of propofol on somatic and visceral pain in subhypnotic doses. Curr Ther Res 1993; 53: 677–81.
Concas A, Santoro G, Serra M, Sanna E, Biggio G. Neurochemical action of the general anaesthetic propofol on the chloride ion channel coupled with GABAA receptors. Brain Res 1991; 542: 225–32.
Nadeson R, Goodchild CS. Antinociceptive properties of propofol: involvement of spinal cord γ-aminobutyric acidA receptors. J Pharmacol Exp Ther 1997; 283: 1181–6.
Jewett BA, Gibbs LM, Tarasiuk A, Kendig JJ. Propofol and barbiturate depression of spinal nociceptive neurotransmission. Anesthesiology 1992; 77: 1148–54.
Puig S, Sorkin LS. Formalin-evoked activity in identified primary afferent fibers: systemic lidocaine suppresses phase-2 activity. Pain 1996; 64: 345–55.
Iwasaki H, Collins JG, Namiki A, et al. Comparison of the effect of propofol and that of pentobarbital on behavioral responses to somatic and visceral stimuli in rats (Japanese). Masui 1991; 40: 1308–13.
Zancy JP, Coalson DW, Young CJ, et al. Propofol at conscious sedation doses produces mild analgesia to cold pressor-induced pain in healthy volunteers. J Clin Anesth 1996; 8: 469–74.
Canavero S, Bonicalzi V, Pagni CA, et al. Propofol analgesia in central pain: preliminary clinical observations. J Neurol 1995; 242: 561–7.
Briggs LP, Dundee JW, Bahar M, Clarke RS. Comparison of the effect of diisopropyl phenol (ICI 35 868) and thiopentone on response to somatic pain. Br J Anaesth 1982; 54: 307–11.
Wilder-Smith OH, Kolletzki M, Wilder-Smith CH. Sedation with intravenous infusions of propofol or thiopentone. Effects on pain perception. Anaesthesia 1995; 50: 218–22.
Petersen-Felix S, Arendt-Nielsen L, Bak P, Fischer M, Zbinden AM. Psychophysical and electrophysiological responses to experimental pain may be influenced by sedation: comparison of the effects of a hypnotic (propofol) and an analgesic (alfentanil). Br J Anaesth 1996; 77: 165–71.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nishiyama, T., Matsukawa, T. & Hanaoka, K. Intrathecal propofol has analgesic effects on inflammation-induced pain in rats. Can J Anesth 51, 899–904 (2004). https://doi.org/10.1007/BF03018887
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03018887